Courtesy: Prof Wolf Petersen, Berlin, Germany
Understanding Meniscus Anatomy and Function
- Medial and lateral meniscus serve as a movable joint surface.
- Contributes to load transmission and joint stabilization.
- Meniscal loss leads to joint overload, resulting in osteoarthritis.
- Importance of meniscus preservation to prevent cartilage damage and osteoarthritis.
Importance of Meniscus Repair in ACL Injuries
- ACL injuries often involve associated meniscal, cartilage, and ligament damage.
- Untreated meniscal injuries increase the risk of post-traumatic osteoarthritis.
- Meniscus repair during ACL reconstruction enhances long-term joint stability.
Meniscus Healing Potential and Repair Criteria
- Healing potential depends on vascular supply:
- Red Zone: Good blood supply, higher healing potential.
- White Zone: Avascular, poor healing potential.
- Favorable repair criteria:
- Tears in vascular zones.
- Longitudinal tears.
- Acute lesions.
- Younger age.
- Contraindications:
- Tears in the white zone.
- Chronic lesions.
- Poor tissue quality.
- Older patient age.
Meniscus Repair Techniques
- Outside-In Technique
- Cost-effective and biomechanically stable.
- Sutures passed through puncture needles and tied at the joint capsule.
- Inside-Out Technique
- Commonly used in the United States.
- Requires specialized instruments and caution to avoid saphenous nerve injury.
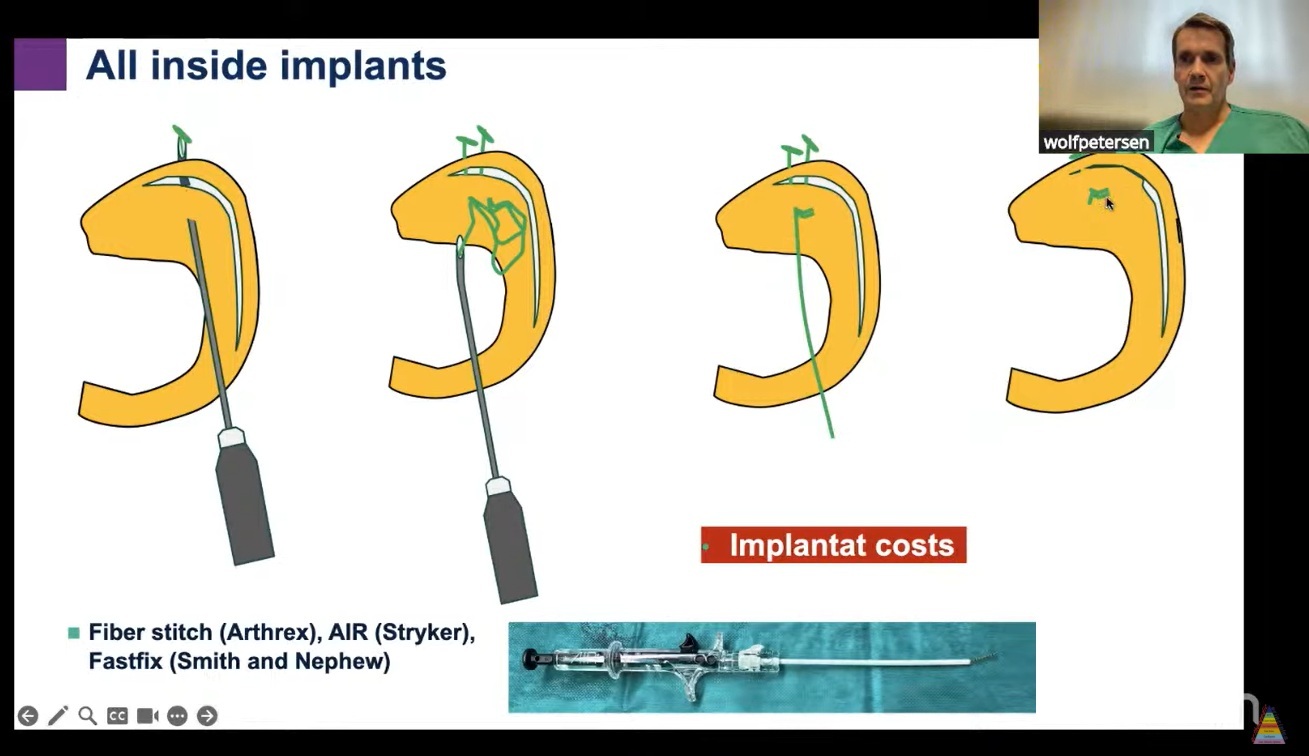
- All-Inside Technique
- Utilizes suture anchors and self-locking knots.
- Minimizes nerve injury risk.
- Preferred for posterior meniscal tears.
Hybrid Repair Approach
- Combination of different techniques for various meniscal zones:
- Posterior part: All-inside technique.
- Intermediate part: Inside-out or outside-in technique.
- Anterior part: Outside-in technique.
Long-Term Outcomes and Failure Rates
- 22% failure rate after 10 years.
- Bucket-handle tears show the highest failure rates (up to 50%).
- Techniques to improve healing:
- Microfracture in the notch.
- Biological augmentation with growth factors.
- Combined ACL reconstruction reduces failure rates due to better stability and biological factors.
Special Considerations for Ramp and Root Lesions
- Ramp Lesions:
- Tears in the menisco-capsular and menisco-tibial ligaments.
- Often missed on MRI; requires arthroscopic probing through the posteromedial portal.
- Stable ramp lesions: Conservative management.
- Unstable ramp lesions: Suture hook repair preferred over all-inside anchor repair.
- Meniscal Root Tears:
- Avulsion or radial tear within 5 mm of the insertion.
- Medial root tears: Degenerative, common in older patients with varus deformity.
- Lateral root tears: Traumatic, associated with ACL injuries.
- Diagnosis aided by MRI signs:
- Ghost sign, meniscal extrusion, and subchondral bone edema.
- Meniscal Root Repair:
- Trans-tibial pullout technique using a cortical button or interference screw.
- Centralization may be required to reduce extrusion.
- Combined high tibial osteotomy (HTO) and root repair recommended for patients with varus deformity and minimal osteoarthritis.
Rehabilitation Protocols
- Rehabilitation varies based on tear type and repair technique:
- Smaller tears (<20 mm): Gradual weight-bearing and range of motion.
- Larger or complex tears: Restricted weight-bearing to optimize healing.
- For ACL reconstruction with longitudinal tears >20 mm:
- 4 weeks partial weight-bearing, ROM restricted to 0–60°.
- Additional 2 weeks, ROM increased to 0–90°.
- Isolated bucket handle tears:
- 6 weeks partial weight-bearing.
- 4 weeks ROM 0–60° and 2 weeks up to 90°.
- Medial meniscus root or radial tears:
- 6 weeks of non-weightbearing with ROM restrictions.
Video Demonstration of Meniscus Repair
- Demonstration of bucket-handle tear repair after ACL reconstruction.
- Steps included:
- Debridement and preparation of the tear.
- Microfracture device for peripheral abrasion.
- All-inside fiber stitch technique for anchoring.
- Inside-out technique for intermediate tears.
- Outside-in technique for anterior tears using a vertical suture configuration.
Challenges and Complications
- Persistent pain may result from cystic formation around implants.
- Rare cases may require revision to remove prominent implants or address nerve entrapment.
- Case of CRPS due to saphenous nerve injury highlighted the importance of visualizing the needle path during repairs.
Discussion and Q&A Session
- Addressed visualization challenges of the posterior horn of the medial meniscus in ACL-deficient knees:
- Suggested slight knee flexion (around 30°) and applying valgus stress.
- Cautioned against MCL pie-crusting due to concerns of increasing medial instability.
- Meniscal extrusion discussed as a consequence of:
- Varus deformity.
- Increased load or obesity.
- Highlighted that meniscal extrusion becomes static and irreversible without intervention.
Conclusion and Future Initiatives
- Emphasis on meniscus preservation to prevent long-term complications and maintain knee stability.
- Professor Petersen expressed enthusiasm about future collaborations and educational initiatives.
Leave a Reply