Courtesy:
Dr Thomas Quin Throckmorton,
Campbell Clinic Professor,
Chief Editor- #AAOS-OrthoInfo
REVERSE SHOULDER ARTHROPLASTY
Birth of the Modern RSA
” Paul Grammont, Lyon France, 1980’s
- Constrained shoulder with medialized center of rotation
- Converts shear forces to compressive forces across glenoid implant – bone interface
Outcomes
• Average forward elevation 100-134 degrees
• Patients do not achieve full ROM afforded by prosthesis
• Limitation likely due to decreased ability to generate muscle force in
cuff-deficient shoulder
Complications
• Notching
• Glenoid lucencies
• Hematoma
• Instability
• Infection
• Revision rate 10%
• Re-operation rate 3.5%
• Instability
• Baseplate loosening/failure
• Component dissociation (rare)
• Deltoid fatigue/strain
• Scapular fractures
Acromion, Scapular spine
• Periprosthetic fracture
• Infection
• Scapular notching
44%-96%
Now usually 15% or les
DECREASING OVER TIME
• Range 0%-68%
• Initially, a reported 50% Complication rate and 33% Reoperation rate
• Then 17% complication rate
• Now 6% (published)
LEARNING CURVE
• Intra-operative complications decrease with increasing experience
• Minimum of 18 cases before “proficiency point” is reached
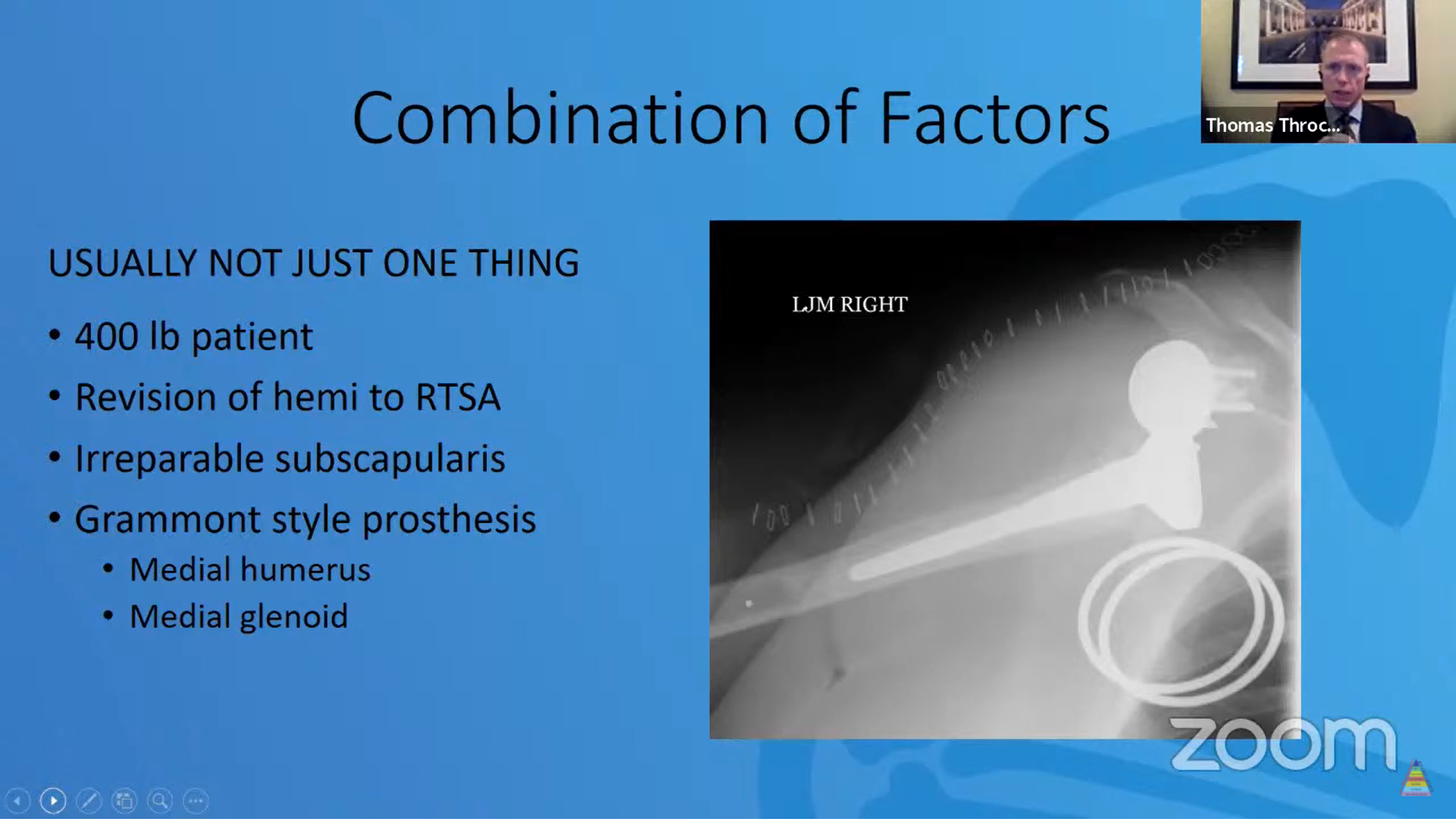
INSTABILITY
• Instability after RTSA is an Uncommon, but complex Problem
• Most series cite a 1-5% Dislocation rate
• Usually within 3 months of Surgery
• Traumatic: Usually fall or low energy Mechanism
• Atraumatic
*Factors
PROSTHETIC (PROTECTIVE)
• Implant lateralization
Glenoid and/or humerus
• Larger glenospheres
• Constrained liners
• Inferior baseplate tilt
• Inferior glenosphere offset
PATIENT (PREDICTIVE)
• Irreparable subscapularis
• Fracture sequelae indication (up to 28%)
• Revision
• Male
• BMI> 30
• Inadequate deltoid tension
• Infection
Causes
• Loss of compression
• Deltoid dysfunction
• Deltoid undertensioning
• Irreparable subscapularis
• Loss of containment
• Mechanical failure
• Impingement
• Bony or soft tissue
Treatment
CLOSED REDUCTION
• Successful 0-62%
• Recreate intraoperative reduction maneuver: Axial traction and flexion
• Treat in abduction orthosis
REVISION SURGERY
• Understand, then address the Underlying cause
• CT scan
• EMG
• Success 50-72%
Up to 45% require additional surgery to obtain stability
Technical Tips
INADEQUATE TENSION
• Mostly done on the humeral Side
• Upsize to obtain “optimal” Deltoid tension
• Lateralized humerus systems will also increase offset through Bearing surface
GLENOSPHERE
• Increase inferior offset
• Increase diameter
• Increase lateral offset
MECHANICAL IMPINGEMENT
Humerus
• Retain stem if possible
• Convertible systems helpful
• Obtain implant record
• Lateralized humerus -can increase Offset
Glenoid
• THOROUGH posterior soft tissue Debridement
• Increase diameter and/or offset
• Debride HO and other impinging Lesions
• Post-implantation stability and Impingement checks
BASEPLATE FAILURE
• Rare
• 0.9% in primary arthroplasty
• 3.6% for revisions
• Lowest incidence in RTSA for PHF
• Highest incidence for OA with Glenoid bone loss
• No difference in incidence Between medialized or Lateralized systems
• Patients with inflammatory Arthritis and advanced glenoid Bone loss underwent volumetric Glenoid analysis with 3D CT scans
• Glenoid bone volumes compared For patients with and without Baseplate failure
Thresholds of glenoid bone Volume CAN predict baseplate failure With non-custom, center-screw Components
• 5cc or less of glenoid volume in females leads to 100 % failure rates
• 14cc or less in males leads to 100 % failure rates
Options for treatment
• Revision RTSA with glenoid bone Grafting
• Impaction versus structural
• Custom or patient-matched Glenoid components
• Revision to hemiarthroplasty
• Resection arthroplasty
DELTOID COMPLICATIONS
• Thought to be from repetitive Stretch and lengthening of the Deltoid
• Forward Elevation and abduction loss averages 0.8 degrees per year
• No significant decline at mid- Term (>5 year) follow up
Biomechanical Study
• Increasing inferior offset in RTSA Constructs increases stretch forces On the deltoid, resulting in a diminished ability of the deltoid to further elongate under physiologic Loads
• Inflection point between 17.3-33mm Of lengthening
• Most pronounced when the Inferior offset exceeds 2.5 mm
• This configuration also significantly decreases the yield displacement Of the construct.
Clinical Study
• Deltoid elongation beyond 25mm associated with increased Risk of deltoid complications like Deltoid strains, Deltoid dehiscence, Acromial fractures,
Muscle/tendon strains without Dehiscence or fracture respond well to Physiotherapy and muscle relaxers
SCAPULAR FRACTURES
• 4% incidence
• Usually within 1 year of Surgery
• Most highly associated with Severe rotator cuff disease
DELTOID WORK
• Glenoid lateralization increases Deltoid work and joint loads for Abduction
• Decreased with humeral Lateralization
• Deltoid less efficient in forward Elevation with glenoid Lateralization also
ACROMIAL STRESSES
• Glenosphere lateralization increases acromial stress by 17%
• Humeral lateralization – 1.7%
• Inferior positioning of glenosphere also decreases stresses (~2.5%)
• Potential implications for acromion And scapular fracture risk
• Stresses highest in the region of most Common acromial fracture site
• Treatment historically felt to be Non-operative
• Lack of studies to validate Surgical technique
• Anecdotal reports of high failure Rates
• Poor clinical results
• More recently, double plating Techniques have been advocated
PERIPROSTHETIC FRACTURES
• 3.5% incidence of humeral Periprosthetic fractures after Primary RTSA
• Treatment traditionally adopted from algorithms taken from total hip arthroplasty
• Non-operative treatment Reported to be viable
• Other sources suggest Conservative treatment “rarely Indicated”
Periprosthetic Fractures Treatment options
• Conservative
• ORIF
• Revision of Humeral stem
• Long stem
• Endoprosthesis
INFECTION
• Notoriously difficult to diagnose in Shoulder arthroplasty
• Low virulence organisms
• Cutibacterium Acnes
• Coagulase negative staph
• Most common symptom is Unexplained pain
• No standardized methodology for Diagnosis or treatment
2018 International Consensus on Management (ICM) of Periprosthetic Infection is u useful algorithm
One study focussed on the ICM Phily Criteria where 96 revision arthroplasties was Identified
• 13 patients treated as infected
• 8 patients were identified by Scoring system as probable Infections
• 3 patients were identified as Definite infections
• 1 and 2 stage Reconstructions have been Described
Systematic review of 287 Shoulders
• 88.5% clearance rate
• Debridement alone- 29.7%
Failure
• 1 stage revision -4% failure
• Significantly better than 2 Stage revisions (14.3% failure)
NOTCHING
CAUSE
• Impingement of polyethylene Bearing surface on inferior
Scapula during adduction
• Osteolytic reaction
• Results in inferior clinical Outcomes at intermediate- Term follow-up
FACTORS
• Glenosphere height
• Inferior glenoid “overhang”
• Inferior glenosphere tilt
• 10-15 degrees
• Humeral neck-shaft angle
• Lateralized center of Rotation
Summary
• The complication rate for reverse total shoulder arthroplasty Continues to improve
• Some complications are best treated by avoidance as treatments for them continue to evolve: FOR EG., Deltoid complications, Scapular fractures, Notching
Others have options more amenable to surgical treatment (FOR EG., Instability, Baseplate failure, Periprosthetic fractures, Infection)
Leave a Reply