Courtesy: Yogesh Joshi, MS Orth, MSc, FRCS Orth
Total Knee Replacement
Technical Goals
– To Restore mechanical alignment of the lower limb
– To Restore joint line
– Balanced ligaments
– To gain Normal Q angle for normal patello-femoral tracking
Position
-Patient positioned supine with knee flexed to 90 degree
-Side support- to hold the thigh in place
-Foot support- to keep the knee flexed(can use 2 foot supports to change angle of knee intraoperatively)
Incisions
Medial Parapatellar Approach
-Advantages
1.Familiar to most
2. Excellent exposure even in challenging cases
-Disadvantages
1.Failure of medial capsular repair
2.Lateral patellar subluxation
3.Access to lateral retinaculum less direct
4.May jeopardize patellar circulation if lateral release is performed
Lateral parapatellar approach
- Can be used in severe Valgus knee
- allows access to lateral side of knee
- Allows easier release of lateral soft tissues
- Technically quite demanding
- Medial patellar eversion is difficult
- difficult to gauge the tibial rotation
Midvastus approach
- Spares VMO insertion
Advantages
- Accelerated rehabilitation (can be used in unicompartmental knee replacement surgeries)
- Improved patellar tracking
Disadvantages
- Less extensile
- Difficult in obese or patients with flexion contractures.
Subvastus approach
Vastus medialis is lifted off the lateral intermuscular septum
Advantages
- Can start early rehabilitation because of Intact quadriceps
- Preserved vascularity of patella
Disadvantages
- Least extensile to the lateral side
- Denervation of VMO possible
Other extensile approaches
• Quad snip approach
• V-Y turndown approach
• Tibial tubercle osteotomy
Preparation of femur
- Entry Point-is slightly medial to the midpoint of the femoral condyles, because the axis of femur exits on the medial aspect of knee.
- Femoral Valgus cut angle= AAF-MAF (ANATOMICAL AXIS OF FEMUR-MECHANICAL AXIS OF FEMUR.
- It is around 5-7 Degrees commonly (can differ in different people-in taller people it is lesser & in shorter people more)
- We use intramedullary guide for femoral cut.
– “Overdrilling’
– Irrigation and evacuation
– Less sclerotic side first - If Flexion contracture is there, can be corrected by excess distal femoral cut.
- Usually the distal femoral cut is taken according to the thickness of femoral component
Anterior, posterior & Chamfer cuts of distal femur
- Native posterior condyle of femur in 3 degrees valgus
- Native tibial plateau in 3 degrees varus
- Anterior and posterior cut is important in getting the rotation of distal femur correct
- Anterior femur cut & posterior condyle cut should be parallel to the tibial cut to maintain neutral rotation
- notching will cause Increased risk of periprosthetic fracture
- “Grand Piano” sign- the standard anterior cut will make a grand piano sign over femur.
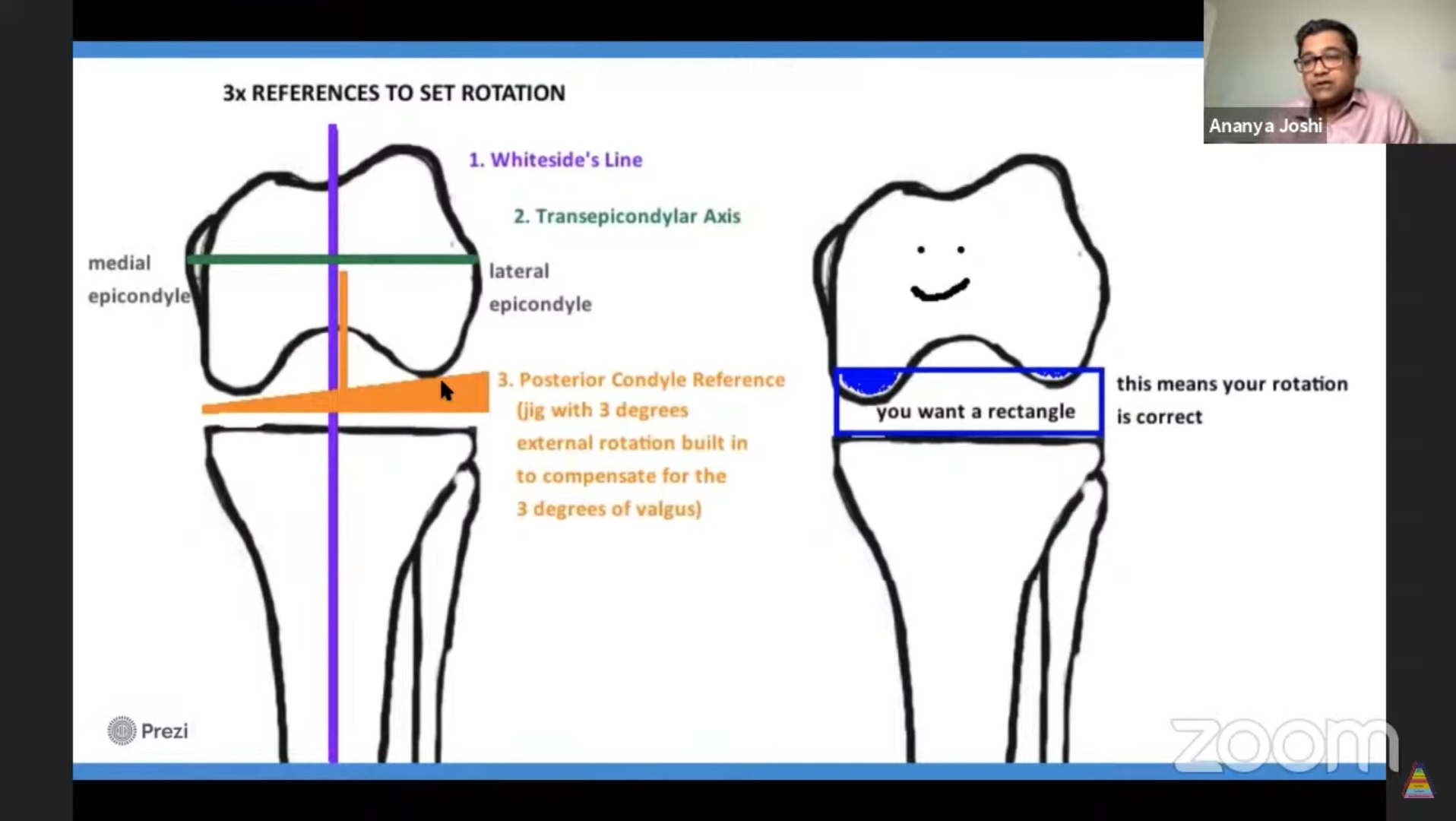
3 references to set rotation
1. Whiteside’s line
2. Trans-epicondylar axis
3. Posterior condylar reference
ROTATION is DETERMINED BY ANTERIOR & POSTERIOR CUT
- The relation between Whiteside’s Line and Transepicondylar Axis will be perpendicular.
- Posterior Condyle Reference (jig with 3 degrees external rotation built in to compensate for the 3 degrees of valgus)
- We need a rectangular flexion gap-which means our rotation is correct.
IMPLANT SIZE
- The size of the implant is based on the AP diameter
- The medio- lateral diameter is unrelated (although there are some companies with “gender specific knee” which means there is a wide and narrow option for each implant size
- The measuring guide sits behind the posterior femoral condyles and the anterior stylus is adjusted to sit nicely on the anterior cortex. This boom is attached to a measuring stick that lines up with a number on the device to give a size
- The 4-in-1 CUTTING JIG is made in every implant size, once you measure the femur size you get the corresponding cutting jig
Tibial Cut
- Angle between AAT and MAT
- Tibial cut angle is Zero
- Tibial deformity is corrected by cutting perpendicular to Mechanical Axis of the Tibia
- Intra or extramedullary guide can be used for tibia
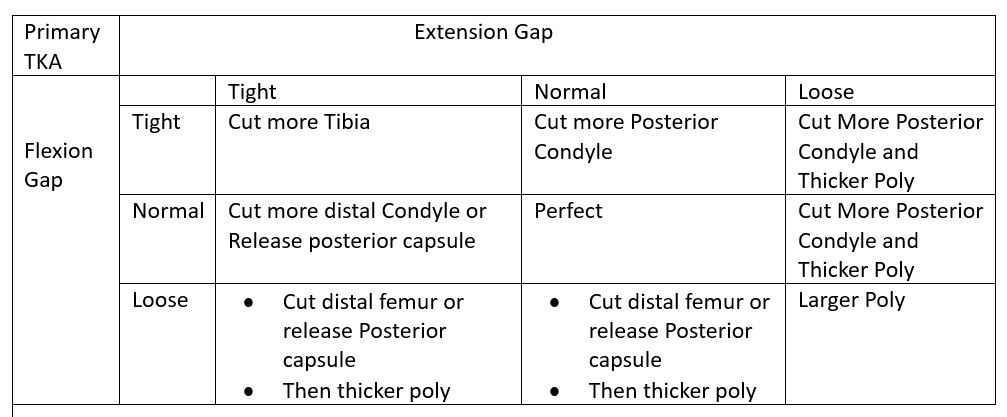
Balancing
- Goal: To make a symmetric rectangle gap (flexion and extension)
- Started with the extension gap followed by the flexion gap
Asymmetric-
1)Bony causes
2)Soft tissue causes
In a varus knee, If gap is not sufficient on medial side
- Clear the osteophytes
- Release Deep MCL
- Release Semimembranosus tendon, posteromedial capsule
- Superficial MCL (anterior part release relaxes the gap in flexion and posterior fibre release relaxes the gap in extension)
If still not corrected,
-Can release pes anserinus
-Subtraction osteotomy of medial tibial plateau
-Pie crusting of MCL as last resort
In valgus knee correction
-Pie crusting of iliotibial band
-Release the posterolateral capsule
-Release PCL and Popliteus tendon.
Tibial Component
4 landmarks while placing the tibial component
1. Medial 3rd of tibia
2. Anteromedial curvature of tibia
3. Transtibial axis
4. Akagi’s line (arises from insertion site of PCL to medial border of patellar tendon)
-Internal rotation of tibia will increase the Q angle and cause patellofemoral issues postoperatively
-Internal rotation tibial component= External rotation of tibial tubercle
-Tibial implant should line up over medial half of tibial tubercle
Patello Femoral Joint alignment
- Maintain the Q angle for patella femoral alignment.
Q angle is increased by
- Internal rotation of femoral component
- Medialising femoral component
- Internal rotation of tibial component
- Lateralising Patellar button
- Increase in Q angle will reduce the stability of PFJ, so better to avoid these things
Patellar component
- Should be Centre or medialized
- Avoid lateralizing of patella, Because, it will Increase Q angle and cause maltracking of patella
Patella
- Restore composite thickness after symmetric resection of patella
- Remove a part of lateral facet because it articulates with the metallic femoral component and produce retinacular pain later on.
- Always check Tracking of the patella.
Cementing
- Clean and dry bone surfaces
- Finger pressurise cement to the bone
- Always Coat Cement over the implant
- Avoid cement to the posterior femoral condyle, because it may reach the posterior recess which is very difficult to remove.
Leave a Reply