Courtesy: Prof Nabil Ebraheim, University of Toledo, Ohio, USA
GROWTH PLATE ANATOMY AND ITS FUNCTIONS
INTRODUCTION
- The growth plate, also known as the physis, is the cartilaginous portion at the ends of long bones where longitudinal growth of the bone takes place.
- This region of bone is characterized by high metabolic activity and is under the regulatory control of a wide variety of hormones and signalling compounds.
- Hormonal regulation of the growth plate can be affected by trauma, medications, and other extrinsic variables causing growth plate abnormalities and subsequent growth disturbances
STRUCTURAL COMPOSITION
The maturation of chondrocytes in the physis is classically divided into five phases .
- Resting phase
- Proliferative phase
- Prehypertrophic phase
- Hypertrophic phase
- Terminal phase
GERMINAL (RESTING) ZONE:
- Contains chondrocytes in quisence
- Replenishes proliferative zone
- Injury causes cessation of growth
PROLIFERATIVE ZONE:
- Contains chondrocytes in mitosis
- Has abundant blood supply
- Responsible for increase in bone length
- Injury causes cessation of growth
HYPERTROPHIC (MATURATION) ZONE:
- Cells accumulate glycogen/lipids
- Weakest zone and site of physeal fractures
ZONE OF CALCIFICATION:
- Mineralisation of matrix
- Infiltration by metaphyseal blood vessels
PHYSEAL INJURY
- Fracture through growth plate.
- Unique to paediatric patients.
- Prevalence – 10-30% of childhood fractures.
- Age – bimodal peaks
- Infancy, 10-12 years of age
- commonest sites –
Distal femur
Distal tibia
Proximal tibia/fibula
Distal radius
ETIOLOGY
- Trauma
- Infection
- Tumor
- Vascular
- Repetitive stress
- Irradiation
CLINICAL PRESENTATION
- History:
- Pain/swelling around the affected joint
- Upper limb – function limited by pain.
- Lower limb – inability to bear weight on affected limb.
- History of trauma.
On examination:
- Swelling +
- Deformity +/- (minimal if present)
- Focal tenderness over physis +
- Limited range of motion of joint
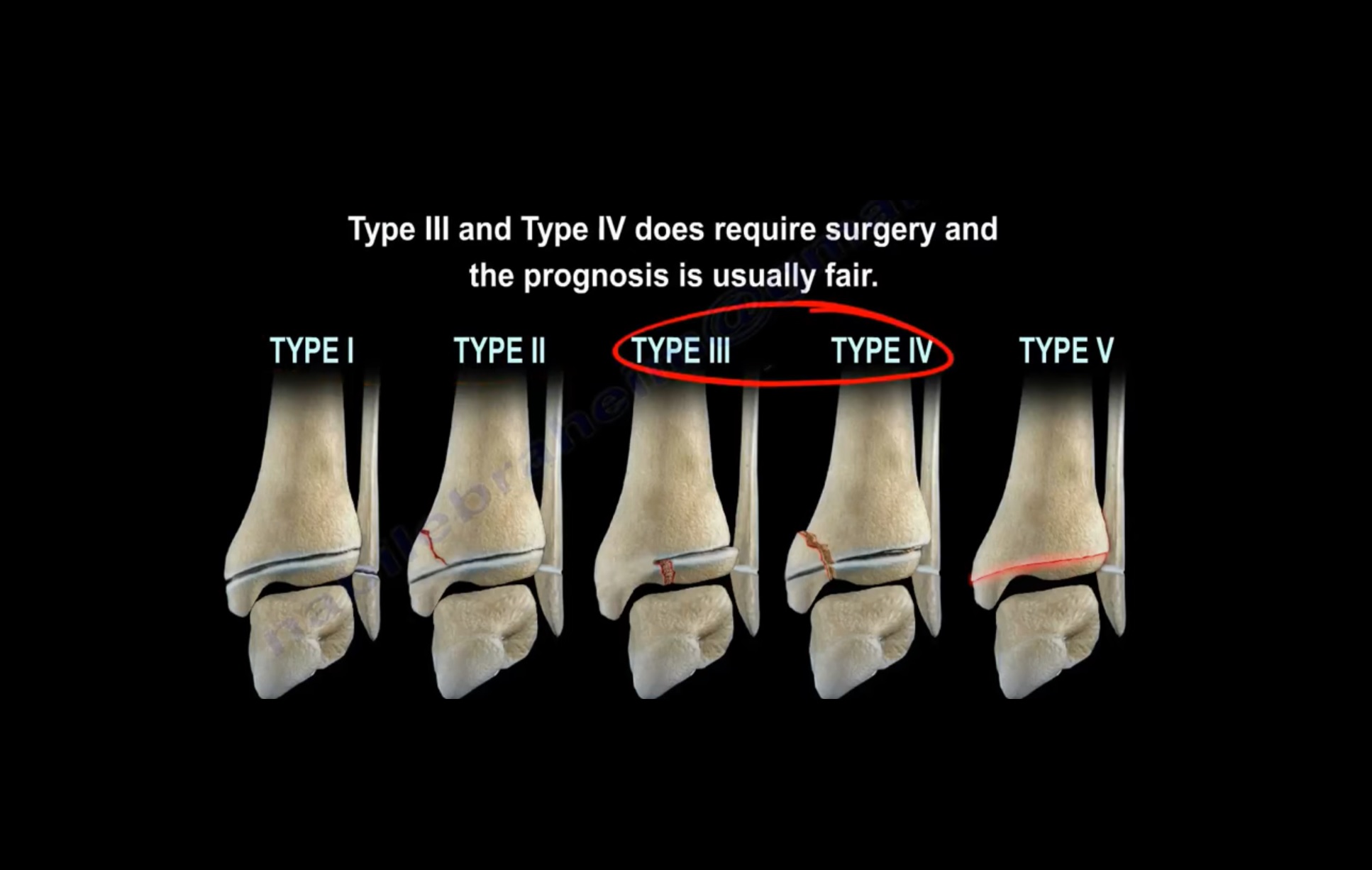
SALTER-HARRIS CLASSIFICATION (1963)
- Type 1 – transverse fracture through the growth plate (6%)
- Type 2 – fracture through the growth plate and metaphysis, sparing the epiphysis (75%
- Type 3 – fracture through growth-plate and epiphysis, sparing the metaphysis (8%)
- Type 4 – fracture through growth-plate, metaphysis and epiphysis (10%)
- Type 5 – compression fracture of the growth plate(1%)
TYPE 1
- A transverse fracture through the physis.
- Physeal separation without any bony injury.
- The growing zone is not injured, so growth disturbance is uncommon.
- Clinically – point tenderness over the epiphyseal plate with swelling.
- X-ray is normal, except widening of physeal plate.
TYPE 2
- The most common type
- Fracture occurs through the physis and metaphysis; epiphysis is spared.
- The metaphyseal fragment is sometimes called the ‘Thurston-Holland fragment.
- Limited growth disturbance; may cause minimal shortening.
TYPE 3
- Fracture through the physis and epiphysis, metaphysis is spared.
- Prone to chronic disability, because it extends into the articular surface of the bone.
- However, rarely results in significant deformity.
- Anatomic reduction (usually open) and stabilization.
TYPE 4
- Involves all 3 elements of the bone, passing through the epiphysis, physis, and metaphysis.
- An intra-articular fracture; thus, it can result in chronic disability.
- Interfere with the growing layer of cartilage cells.
- Can cause premature focal fusion of the involved bone leading to deformity of the joint.
- Frequent around the medial malleolus, lateral condyle.
- Anatomic reduction and adequate stabilization.
TYPE 5
- A compression or crush injury of the physis, with no associated epiphyseal or metaphyseal fracture.
- The clinical history is of paramount importance.
- A typical history of an Axial load Injury.
- X-ray at the time of injury shows no abnormality.
- Usually diagnosed retrospectively. (Minimum 6 months)
- Worst prognosis
MANAGEMENT
- After thorough history and clinical examination.
X-ray: - It is difficult to assess as the physis is radiolucent and the epiphysis is incompletely ossified.
On x-ray:- - The physeal widening of the gap
- Tilting of the epiphysis
- Compare the injured side with the normal
- Repeating x ray within few days
CT Scan:
- To visualize fracture anatomy in severely comminuted fractures epiphysis and metaphysis
MRI Scan
- Most accurate for fracture anatomy if done in acute period
- Identifies formation of bony bridge earlier than x-rays
PLAN OF MANAGEMENT DEPENDS ON
- Severity of the injury
- Anatomic location of the injury
- Classification of the fracture
- Plane of the deformity
- Patient age
- Growth potential of the involved physis
TREATMENT
FOR TYPES 1 & 2
- Closed reduction and immobilization in cast is done usually
- Gentle reduction.
- Never forceful and repeated. Reduce as soon as possible
- Acute injuries must be immobilised in a slab, so as to allow some swelling from the fracture.
- Repeat radiographs at weekly intervals to document
- Maintenance of acceptable position until early bone healing.
SH type 1 injury managed with Percutaneous K-wires
SH type 2 managed with CC screws
SH type 3 managed with canulated screws
SH type 4 – Cannulated screw fixation
FOR TYPES 3 & 4:
- Require anatomical realignment via ORIF
- ORIF can be with lag screws or k-wires running parallel to physis
FOR TYPE 5:
- Usually diagnosed retrospectively
- However high index of suspicion must be maintained in high risk injuries
SURGICAL METHODS:
- Bone bridge resection with fat interposition.
- Bone bridge leads to angular deformity.
- Interposition of fat prevents bone bridge formation.
- Ipsilateral completion of arrest
- Contralateral epiphysiodesis
- Limb lengthening
- Corrective osteotomy
BONE-BRIDGE RESECTION WITH FAT INTERPOSITION:-
- Type V fractures are rarely diagnosed acutely, and unfortunately, treatment is often delayed until the formation of a Bony bar across the physis is evident.
- Saucer and cup appearance.
- Angular deformity.
Materials used for interposition are
- Fat
- Bone wax
- Silicon rubber
- Polymethylmethacrylate
FOLLOW UP
- Check x-ray post-reduction.
- Re-evaluated in the short term (7-10 days) to ensure maintenance of reduction.
- Weekly follow-up till callus appears on x-ray.
- After initial fracture healing has occurred, physeal fractures require additional follow-up x-rays 6 months and 12 months after injury to assess for growth disturbance.
- May be extended up to 2 years.
2 phases:
ensuring bone healing
monitoring growth
REHABILITATION
- Types 1 and 2 fractures are immobilized for 3 – 6 weeks
- Types 3 and 4 fractures are immobilized for 4 – 8 weeks
- Patient resumes unrestricted physical activities 4 – 6 weeks following removal of implants for fractures that required operative fixation.
- Then gradually, ROM exercises are started.
PROGNOSIS
- Severity of the injury
- Age of patient at time of injury
- Type of fracture
COMPLICATIONS
- Growth arrest:
- Due to disruption of physeal blood supply or bone bridge formation.
- Complete arrest leads to shortening/LLD
- Partial arrest leads to angulation
- Growth acceleration
- Secondary osteoarthritis
Leave a Reply