Courtesy: Satish Dhotare, FRCS Tr and Orth, Liverpool, UK
BIOMECHANICS OF TOTAL HIP ARTHROPLASTY
1) What are the important factors to consider while planning for THR ?
PATIENT FACTORS SURGICAL FACTORS LOCAL/ PROSTHESIS
- Age, Surgical skills, Prosthesis design
- Functional demands, Approach, Templating
- Infections, Technique, implant fixation,
- Neuropathic joints, Survival
- Patients’ compliance, Cost effective
- Obesity,
- Co morbidities,
- Neuromuscular disorders
2)Which are the common approaches used in THR , what are its merits and demerits ?
- Medial
- Direct anterior / smith Peterson
- Anterolateral / Watson jones
- Direct lateral ( Hardinge , Transgluteal)
- Posterolateral ( Moore or southern)
Advantage of Direct Lateral Approach:
a) Reduce the risk of sciatic nerve injury
b) Reduce risk of dislocation
Disadvantages
a) difficult to approach acetabulum
3)Biomechanics of hip in THR – How to reduce the joint reaction force ?
- Fulcrum: Hip Joint
- Lever Arm: Femoral head, neck and trochanter
- Power: Hip Abductor Muscles
DECREASE BODY WEIGHT MOMENT- Reduce body weight, decrease lever arm, medialise the axis of rotation
HELP THE ABDUCTORS
A) Provide additional moments- walking stick in opposite hand, suitcase in ipsilateral hand
B) Increase abductor lever arm- increase offset, osteotomy, Lateral transfer of GT, Varus angulation of stem of THR
IMPROVE ABDUCTOR LINE OF FUNCTION
Major indication for THR- Pain relief and improve the function
5) History
Sir John Charnley revolutionised THA – his principle was LOW FRICTION ARTHROPLASTY
Principles used by him:
a) Increased offset and lever arm of hip joint (improves abductor function and correction of LLD)
b) Lateralisation of abductors
c) Medialisation of COR
6) Factors affecting Frictional torque of THA
Materials of bearing surfaces
Femoral head size
Polyethylene thickness
Peripheral or equatorial vs polar contact
7) Acetabular components
• Acetabular preparation for cemented cup
? No medialisation , anatomical location
? 3 large keyholes to provide stabilisation of bone cement interface
? No need to expose subchondral bone because heat from bone cement will cause sub chondral bone necrosis
? Modern Cups
Flanges – compress cement
Groove- increase surface area and bonding to the cement ( deep grove decrease polyethylene thickness )
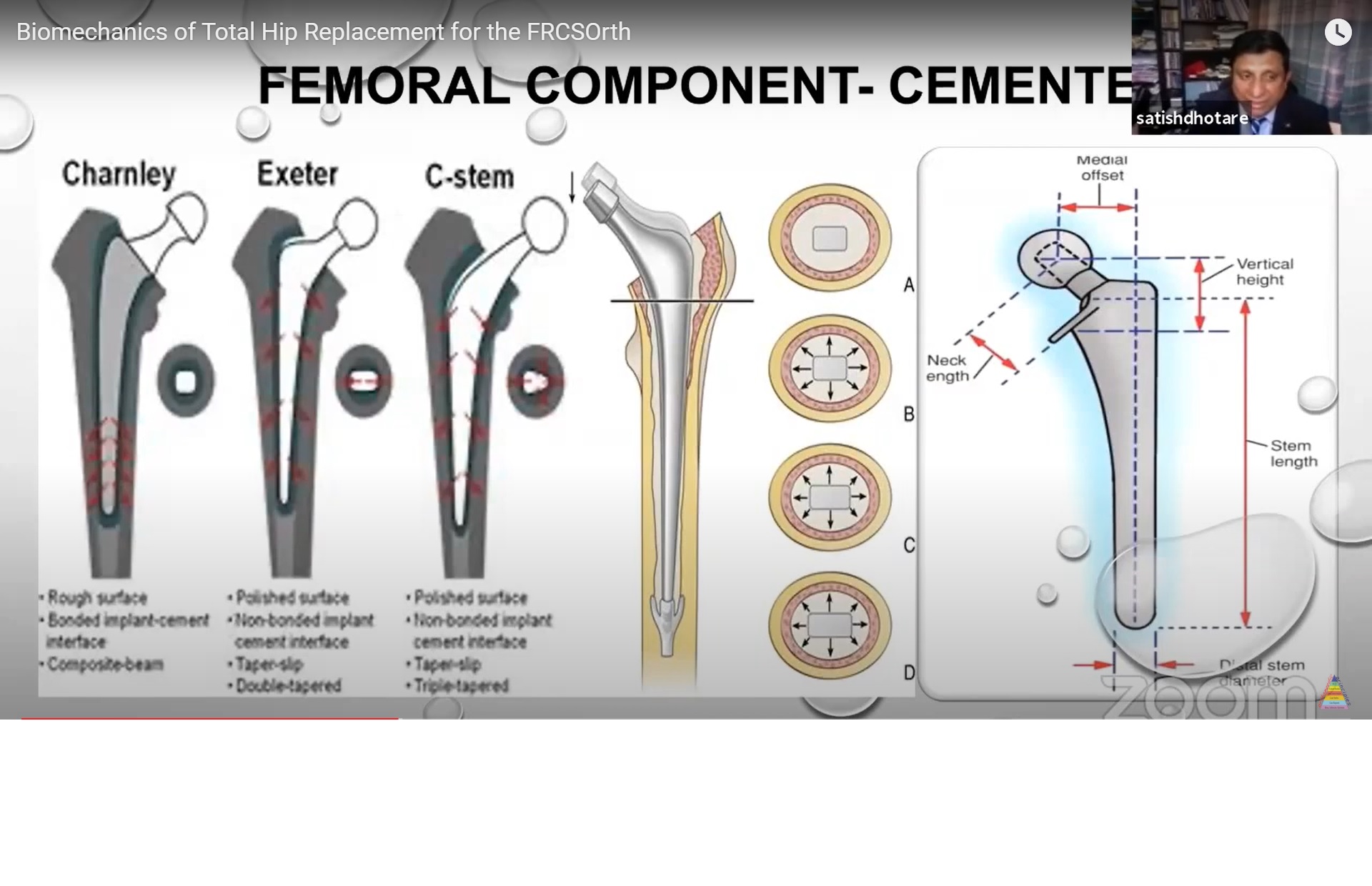
8) FEMORAL COMPONENETS
2 Types
Cemented Stem
a. Charnley’s Stem
– Rough Surface
– Better Bonded Implant – Cement Interface
– Composite Beam
Dis Advantage – Increased Stress And Cement Mantle Breakage Leads To Failure
b. Exeter
-Taper Slip
Double Tapered
Polished Surface
Non-Bonded Implant – Cement Interface
b. C – Stem
-Polished Surface
Taper Slip
Triple Tapered
Nonbonded Implant Cement Interface
Uncemented Stem
Type 1 – Single Wedge
Type 2 – Double Wedge
3 A – Tapered Round
3 B – Tapered Spine /Cone
3 C – Tapered Rectangle
4 – Cylindrical Fully Fully Coated
5- Modular
6 – Anatomic
9 ) BEARING SURFACE
Metal On Metal
Metal On Polyethylene
Ceramic On Polyethylene
Ceramic On Ceramic
10 CEMENTING TECHNIQUEs
First Generation
• Hand Mix With Spatula
• Leave Cancellous Bone
• Vent Femoral Canal
• Minimal Canal Preparation
• Irrigate And Suck Femoral Canal
• Manual Insertion Of Dough
• Manual Insertion Of Stem
• Femoral Stem Shapes
Second Generation
• Hand Mix With Cement Gun
• Remove Bone From Endosteal Surface
• Distal Cement Restrictor
• Brush Pulsatile Irrigation
• Irrigation Pack And Dry
• Cement Gun Insertion
• Manual Position Of Stem
• Improve femur Design
Third Generation
• Vacuum Centrifuge Mixing
• Remove Bone From Endosteal Surface
• Distal Cement Restrictor
• Brush Pulsatile Irrigation
• Irrigation Pack With Adrenaline Gauze And Dry
• Cement Gun Insertion And Pressurisation
• Manual Position Of Stem
• Surface Texture And Contouring
Fourth Generation
– Third Generation Technique with Proximal And Distal Centraliser
11. BARRACKS AND HARRIS GRADING SYSTEM TO ACESS QUALITY OF CEMENTING
Grading Radiographic characteristics
A Complete filling of the medullary canal without radiolucent line between the cement and the bone
B Radiolucent line covering up to 50% of bone cement interface
C Radiolucent line covering between the 50% – 99% of the cement bone interface or incomplete cement mantle
D Complete radiolucent line (100%) at the cement bone interface and /or absence of stem distally to the end of the stem
12. POST THR COMPLICATIONS
A. Painful THA
1) Non hip pain :24 % (spine)
2) Loosening 19%
3) Micro instability
4) Wear
5) Metallosis
B. Complications and indications for revision
1) Most common : Aseptic Loosening (43.5%),
2) Pain (16.9%),
3) Lysis (14.0%)
4) implant wear,
5) Dislocation/subluxation
6) Infection
7) Periprosthetic fracture
8) Implant fracture
9) Adverse reaction to Particulate debris
10) Head/socket size mismatch
C. What is the most common cause for aseptic loosening ?
WEAR
Causes of aspect loosening
A Wear- progressive loss of substance from the material secondary to chemical or mechanical action
1) Adhesion wear ( at the junction between 2 opposing surfaces )
2) Abrasion wear
3) Fatigue wear
B Corrosion
1) Generalised /galvanic
2) Localized :
a.pitting
b.crevice
c.Fretting
d.stress
e.intergranular
f.inclusion
13 What are the Modes of Wear ?
Mode 1 The generation of wear debris with motion between bearing surfaces as intended by the designers
Mode 2 Wear between primary against secondary bearing surface not intended by the designer after excessive wear in mode 1 e.g. A femoral head articulating with a metal acetabular backing following wearing of polyethylene
Mode 3 Refer to wear between two primary bearing surface with in interposed third body particle, called third body wear or abrasion (bone,cement,metal)
Mode 4 Two non-bearing surface (non primary ) rubbing together e.g. Back side wear of an acetabulum liner, fretting and corrosion of modular taper connection and fretting between a metallic substance and fixation screw
14 what is the pathophysiology of osteolysis ?
Wear particles engulfed by Macrophages ? Multiple inflammatory mediator release ?Stimulate osteoclast mediated osteolysis-? Failure
15 MODES OF FAILURE
Mode of cemented stem failure
1) Pistoning stem with cement
• Subsidence of stem in the cement mass
• Stem is displaced distally, producing radiolucent zone & punched out area of cement near the tip of cement mass
• Tip of stem knocks off end of cement mantle & gave off characteristics crack in the cement at the stem tip is instantly recognizable
2) Pistoning -stem/cement within bone
• Subsidence of cement mantle and stem
• Radiolucent zone can be seen about the entire cement mass
3) Medial mid stem pivot
• Proximal medial, distal lateral shift
• Stem rotates around the centre point
• Medial stem pivot caused by medial migration of proximal portion of femoral stem
• Lateral migration of distal tip results from inadequate superomedial & inferolateral cement support
• This may produce a fracture of the cement a mid-stem and of sclerotic bone lateral tip of the stem
4) Calcar Pivot
• Wind shield wiper effect (distal toggle )
• This happens with only non cemented component with large collar ( e.g AMP)
• Distal portion of stem loosens and begins to pivot around the collar
5) Cantilever Bonding ( Fatigue )
• Bending cantilever fatigue ? Proximal loss of stem support with distally stem securely fixed
• Proximal cement breaks up but distal portion of the stem remains tightly fixed in place
• Subsequent medial migration or deformation of proximal stem
• Radiolucent zone develop proximally medial and lateral to the stem and may progress to stem failure.
16) How long do you take to recover from Hip Replacement Surgery?
In general, its around 2- 4 weeks. It all depends on how well you were prior to surgery. If you had good range of motion, and mild pain prior to surgery, your recovery is going to be faster. It also depends on factors like, age, other diseases that you have, your nutritional status and the rehabilitation protocol. A good physiotherapist will help you in the process of recovery.
17) Which method of hip replacement is the best?
There are three different types of total hip replacement: Fully cemented(Femoral and Acetabular side cemented), Fully Uncemented and Hybrid(Cemented femoral and Uncemented Acetabular). While the results of a Fully Cemented and Hybrid technique have similar results, the result of an Uncemented THR is slightly inferior, due the higher incidence of periprosthetic fractures!
18) What is the average age for a Hip Replacement?
Hip replacement may be done at any age over 18 years. Its not recommended in age less than 18 years. It depends on what age you contract the disease. It is wiser to postpone a Hip Replacement as much as possible, because the average life span of a well done Total Hip Replacement is around 15 years, and then you need to revise, if you develop symptoms. Hip Preservation is an evolving field, where you try to preserve the native hip anatomy by procedures like Arthroscopy and osteotomy.
19) Is Hip Replacement a Serious operation?
A hip replacement is a major surgical procedure. A Total Hip Replacement is done when pain killers, physiotherapy do not relieve the pain. A hemi arthroplasty, or a partial hip replacement is a relatively common procedure done in elderly patients who have fractured their hip(neck of femur fracture)
Nice presentation