Courtesy: Yogesh Joshi, Wrexham, UK
Tibial Plateau Fractures
Anatomy
- Tibial plateau consists of medial and lateral plateau separated by the intercondylar eminence
- Medial plateau- larger, lower(concave), stronger.
- Medial plateau fractures occur more often en-bloc and are invariably associated with more severe injuries and fracture dislocations
- Lateral plateau – higher(convex), thicker cartilage.
- Lateral plateau fractures are more common and may include articular depression and fragmentation.
- Tibial slope: 10 degrees posteroinferior
Introduction
- Tibial Plateau fractures are periarticular injuries of the proximal tibia and is frequently associated with soft tissue injury.
- They account for around 1% to 2% of all long bone fractures
- Bimodal age distribution is seen, younger individuals usually get comminuted fractures due to high energy injuries whereas low energy falls are generally the cause in elder population
Mechanism of injury and fracture pattern
- Vector of applied load, amount of energy, and quality of bone determine type of fracture
- Valgus load – lateral plateau
- Varus load – medial plateau
- Axial load – bicondylar
- Combination-fracture dislocation ,high energy, usually medial-sided plateau fractures ,frequently associated with soft tissue injuries
low energy-usually causes lateral plateau fractures
History
• Mechanism of injury – high-energy vs low-energy
• Unable to bear weight after injury
• Baseline functional status
• Comorbidities
Physical examination
• Inspection: look circumferentially to rule-out an open injury. Assess soft-tissues for timing of operative intervention
• Palpation: evaluate for compartment syndrome
• Varus/valgus stress testing: any laxity & more than 10 degrees indicate instability
• Neurovascular exam: perform ankle-brachial index in case of asymmetry in pulses and if ABI10mm articular depression, >6mm condylar widening
• Medial meniscal tear-most commonly associated with Schatzker IV fractures
• ACL injuries-more common in type IV and VI fractures (25%)
• Compartment syndrome
• Neurovascular injury
Fracture classifications
• Schatzker classification
• AO/OTA classification
• Luo three column classification
• Hohl and Moore classification
Schatzker classification
Type I: Split fracture of the lateral plateau
Type II: Split depression fracture of the lateral plateau
Type III: Pure depression fracture of the lateral plateau
Type IV: Medial plateau (possible fracture / dislocation)
Type V: Bicondylar plateau fracture
Type VI: Plateau fracture with metaphyseal/diaphyseal dissociation
AO/OTA Classification
AO / OTA (41- Proximal tibia)
Type A: Extraarticular fracture (41-A)
Type B: Partial articular fracture (41-B)
– B1: Pure split
– B2: Pure depression
– B3: Split depression
Type C: Complete Articular fracture (41-C)
– C1: Simple articular, Simple metaphyseal
– C2: Simple articular, Multi-fragmentary metaphyseal
– C3: Multifragmentary articular
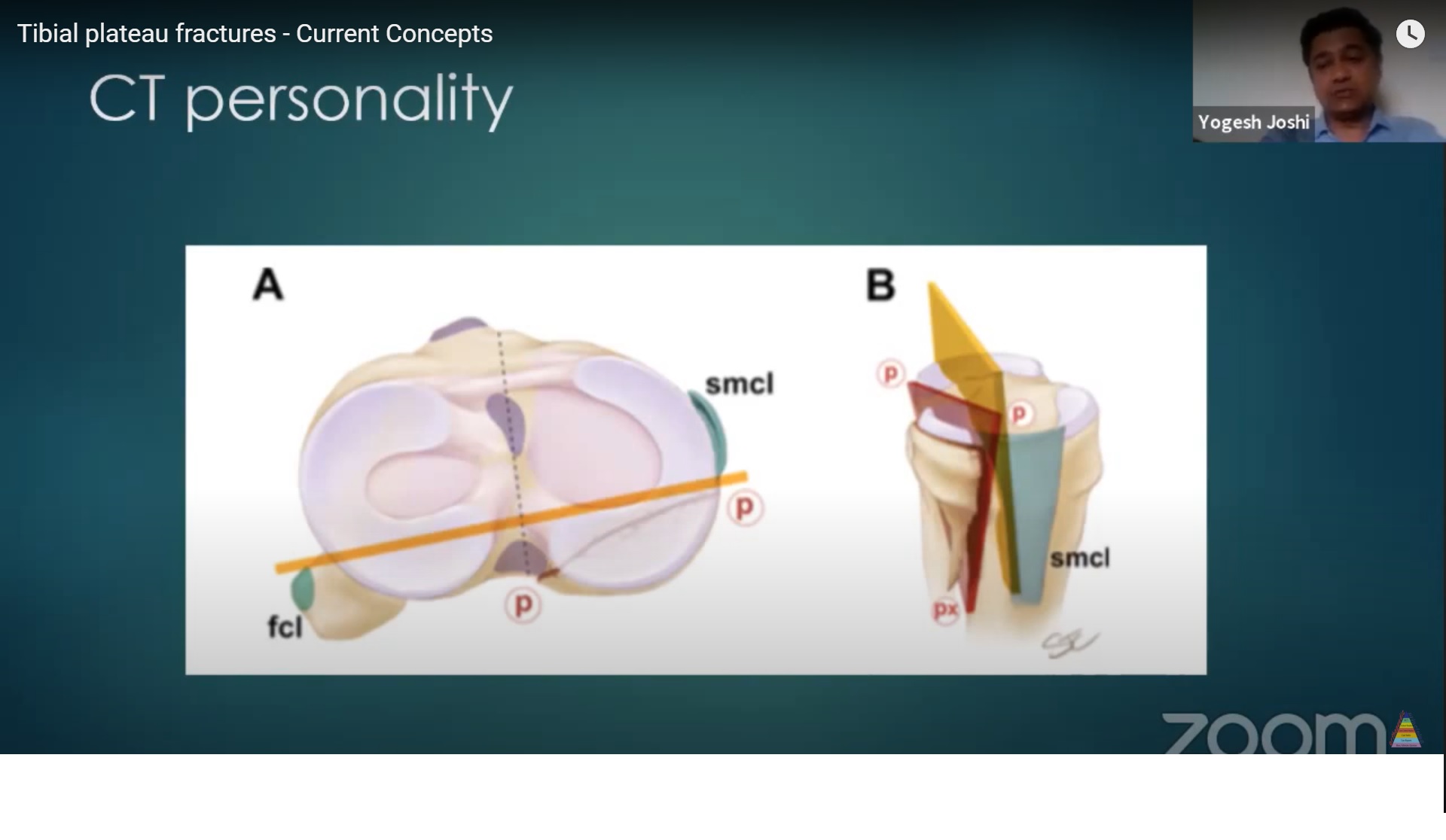
Luo Three-column Classification
- Axial CT based classification
- Divides tibial plateau into 3 columns- medial, lateral and posterior
Hohl and Moore Classification
Type I – split
Type II – entire condyle
Type III – rim avulsion
Type IV – rim compression
Type V – four part
Treatment principles
• Restoration of articular congruity, axial alignment, joint stability, and functional motion
• Fixation must be stable enough to allow early motion and the technique should minimize wound complications
• If depression or displacement exceeds 10 mm, surgery to elevate and restore the joint surface is indicated.
• If the depression is less than 5 mm in stable fractures, nonoperative treatment yields good results
• Studies have shown that posttraumatic arthritis is associated with residual instability or axial malalignment and not the degree of articular depression.
• Instability may result from ligamentous disruption, osseous depression of the articular surface, or translational displacement of a fracture fragment.
• Ligament injuries occur in 10% to 33% of tibial plateau fractures
• The major indication for surgery is not the measure of depression of the fragment or articular surface but the presence of varus or valgus instability of 10 degrees or more with the knee flexed less than 20 degrees.
Non operative treatment
- Cast braces or hinged braces can be used to unload the injured side of the joint.
- They were once commonly used to stabilize the injured joint while permitting some degree of joint mobility.
- Most patients with nonoperatively treated tibial plateau fractures should be kept non–weight-bearing during the initial weeks after injury.
- The duration of non–weight-bearing depends on the fracture pattern but is typically 4 to 8 weeks
Indications:
• non or minimally displaced fractures
• Small depressions of lateral plateau without deformity
• Patients with significant medical comorbidities and elderly with low functional demands
Indications for surgery
• Open fractures
• Fractures with vascular injury or compartment syndrome
• Fracture dislocations
• Displaced intraarticular fractures
• Articular depression causing knee instability
• Malalignment, especially varus
• Polytrauma
Temporary external fixation Indications
• Open fractures
• Acute vascular injury
• Severe, closed soft-tissue injury
• Damage control in polytrauma
Surgical options
Schatzker type I
• Restore articular congruity
• Open vs. percutaneous
• Fixation-Lag screws , Buttress plate
Schatzker type II
• Usually done via anterolateral approach
• Submeniscal arthrotomy for full visualization of articular surface
• Elevate articular depression
• Reduce condylar widening
• Large pelvic reduction clamp ,Temporary K-wires , femoral distractor
• Fill defect – Allograft, Autograft, Bone substitutes
• Buttress plate – Nonlocking: Mostly , Locked: osteoporotic bone
Schatzker type III
• Elevate depressed fragment
• Most recently- inflatable balloons
• Fill defect
• Stabilization – Subchondral screw
Schatzker type IV
• Surgical approach – Posteromedial
• Fixation – with an antiglide plate and interfragmentary screw as appropriate. Straight medial plating/Posteromedial plating /Combination
Schatzker type V & VI
• Dual plating
• Lateral locked plating
• External fixation
Adverse outcomes and complications
- Loss of reduction
- Wound breakdown and infection
- Septic arthritis after external fixation application
- Knee stiffness
- Prominent or painful hardware
- Non-union or delayed union
- Posttraumatic arthritis
Future trends
- Better implants
- Better methods to position implants
- Better methods and materials to fill the void
- Percutaneous soft tissue monitors
- Realtime fluoroscopic 3D imaging techniques
Common Questions:
Can you walk with a Tibial Plateau Fracture?
It is advised that you should not walk if the fracture has happened recently. If fracture is stable and undisplaced and a plaster is applied, the patient can start walking with an assistance within 4- 6 weeks
If the fracture is treated surgically, weight bearing is in similar lines. Toe-touch weight bearing within 4- 6 weeks, around 50% weight bearing in 6-7 weeks and full weight bearing within 3 months. There could some deviation in these general guidelines, based on the stability of fracture.
How long does it take to recover from a tibial plateau fracture?
It takes around 3 months to recover from a tibial plateau fracture
Leave a Reply