Courtesy: Dr Ajith Appuhamy, FRCS Tr and Orth, FEBOT, SriLanka
POLYTRAUMA
DEFINITION: Defined as a syndrome of multiple injuries with systemic traumatic reaction which may lead to dysfunction of organ or vital system.
Polytrauma is a significant injury in at least two of the following body regions ;
- Head, neck and cervical spine
- Face
- Chest and thoracic spine
- Abdomen and lumbar spine
- Limbs and bony pelvis
- External (skin)
- AIS >= 3
ISS > 15 = POLYTRAUMA
LATEST DEFINITION
Expanded to include concurrent injury to two or more body parts or systems that results in cognitive, physical, psychological or psychosocial impairment.
PREVALENCE
- Worldwide – it is the most common cause of death among young age group ( 14-44 years)
- Third most common cause of death in all age groups
MULTIDISCIPLINARY APPROACH
Should include the following as part of team:
Trauma surgeon
Physician
GU surgeon
Intensive care specialist
Physiotherapist
Interventional radiologist
General surgeon
Anesthetic consultant
Orthopedic injuries are generally not life threatening unless they result in significant hemodynamic instability.
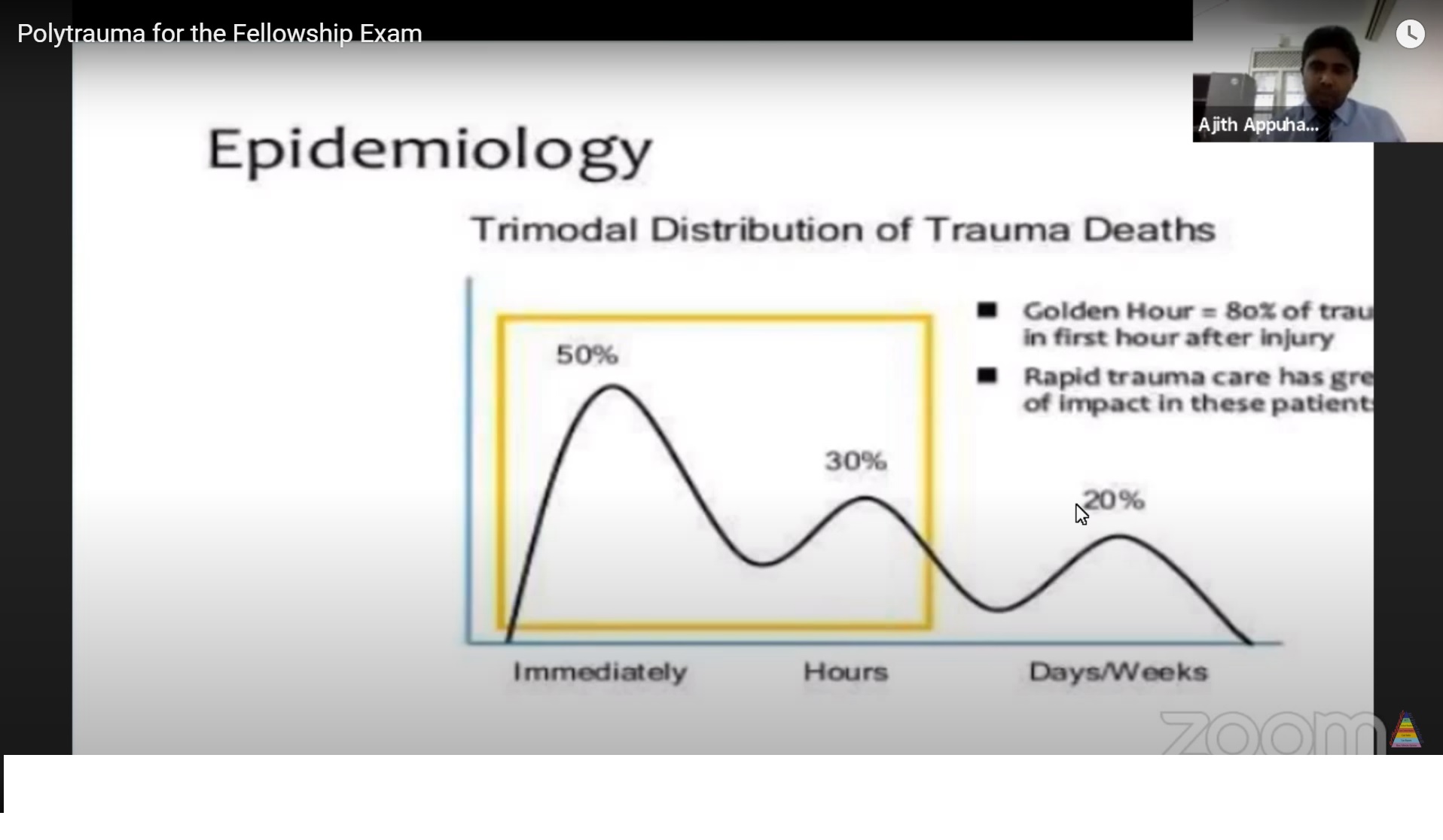
DEATH IN POLYTRAUMA – TRIMODAL DISTRIBUITION OF TRAUMA DEATHS
1. FIRST PEAK OF DEATH
- Immediately
- Major Neurological or Vascular Injury
- 50% OF DEATHS
2. SECOND PEAK OF INJURY
- Within Few Hours
- IntraCranial Hematoma
- Major Abdominal or Thoracic Injury
- 30% OF DEATHS
3. THIRD PEAK OF DEATH
- Days or Weeks
- Sepsis or MultiOrgan Failure
- 20% OF DEATHS
GOLDEN HOUR – 80% OF TRAUMA IN THE FIRST HOUR AFTER INJURY
PATHOPHYSIOLOGY OF TRAUMA
- Whenever an injury occurs, inflammatory response is stimulated.
THE FIRST HIT – THE TRAUMA
- Inflammatory response increases but is confined to the SAFE ZONE.
- With proper resuscitation it comes back to normal.
THE SECOND HIT – THE SURGERY
- 2 to 5 days.
- Inflammatory response is EXAGGERATED.
- Possibility of entering into DANGEROUS ZONE, when once entered reversibility is less likely.
In some individuals the lengthy surgery of early total care exacerbates the systemic inflammatory response resulting in death from MULTIORGAN FAILURE OR ARDS.
TRAUMA TRIAD OF DEATH
Vicious cycle of :
HYPOTHERMIA
COAGULOPATHY
METABOLIC ACIDOSIS
When there is blood loss it results in HYPOTHERMIA that halts the COAGULATION CASCADE resulting in COAGULOPATHY, that can result in METABOLIC ACIDOSIS which will in turn DECREASE THE MYOCARDIAL PERFORMANCE.
GOAL OF MANAGEMENT
Restoration of normal physiology – “Pre-injury status”
PRIORITIES :
1. LIFE SALVAGE
2. LIMB SALVAGE
3. SALVAGE OF TOTAL FUNCTION IF POSSIBLE
LIFE SALVAGE :
- 50 % deaths due to trauma occurs before the patient reaches hospital
- 30 % occurs within 4 hours of reaching the hospital
- 20 % occurs within next 3 weeks in the hospital
- If preventive measures are taken , 70 % deaths can be prevented
- Meaning 30 % deaths are Non – salvageable deaths.
PATIENT ASSESSMENT
ATLS PROTOCOL – 4 inter-related stages
1. Rapid primary survey with simultaneous resuscitation
2. Detailed secondary survey
3. Constant re-evaluation
4. Initiation of definitive care
BOAST GUIDELINES
BRITISH ORTHOPEDIC ASSOCIATION FOR ACUTE MANAGEMENT OF PELVIC FRACTURES.
PARAMEDIC LEVEL ;
Apply pelvic binder if pelvic fracture is suspected.
If hemodynamically unstable, inform and transfer the patient to nearby trauma centre.
Obtain CECT SCAN of CHEST, ABDOMEN AND PELVIS.
Binder can mask many catastrophic pelvic fractures.
Obtain an x-ray after removal of pelvic binder.
PRIMARY HEMOSTATIC RESUSCITATION MEASURES
1. PELVIC BINDER
2. TRANEXAMIC ACID
3. MASSIVE TRANSFUSION PROTOCOL
4. PERMISSIVE HYPOTENSION
AIM :
Initiate clot formation
Maintain the clot
Prevent trauma triad of death
PELVIC BINDER
- Act as a hemostatic device
- Reduction is a bonus ; not the main purpose
- It provides a TAMPONADE EFFECT
- Since venous wall is thinner, pelvic fractures lead to venous bleeding.
- APPLICATION OF PELVIC BINDER: Slightly internal rotate ; the bind should lie on the greater trochanter.
TRANEXAMIC ACID
- Antifibrinolytic action which promotes and stabilizes clot formation
- CRASH – 2 trial – large international, randomized multicentered trial
Benefits :
1. Reduced risk of death in bleeding patients
2. Reduced the risk of mortality
If no contraindications ; 2 grams bolus dose can be given.
Ideally given less than 1 hour after injury
If given more than 3 hours – less effective and could be harmful
MASSIVE TRANSFUSION PROTOCOL
RBC : PLATELET : FFP : CRYOPERCIPITATE – 1 : 1 : 1 : 1
PERMISSIVE HYPOTENSION
- Balance between loosing and infusion
- SBP – 90 mm Hg
- Protect primary clot, maintain it and propogate it
- Avoid ionotropic infusion
- Avoid colloids and crystalloids
CONSTANT EVALUATION
1. GCS
2. BLOOD PRESSURE
3. CLOTTING PROFILE – APTT, PT INR ;
BEDSIDE TESTS like THROMBOELASTOGRAPHY AND ROTATIONAL THROMBOELASTOMETRY
4. Serum lactate
< 2 – ETC 2-2.5 – Marginal > 2.5 – DCO (Latest paper – Vallier – 4 cut off level)
5. Renal profile
6. Urine output
Adult > 1 ml/kg/hr
Children > 0.5 ml/kg/hr
SECONDARY RESUSCITATION MEASURES
After primary resuscitation we classify patients as :
1. GOOD RESPONDER
2. TRANSIENT RESPONDER
3. NON RESPONDER
If GOOD RESPONDER :
- Proceed with management.
- If within 24 hours good responde proceed with ETC.
If TRANSIENT RESPONDER :
- Resuscitate further and watch the trend of the patient.
- If patient improves proceed with ETC.
- If patient deteriorates patient is considered a NON RESPONDER.
If NON RESPONDER :
INTERVENTIONAL RADIOLOGIST should be informed.
1. ANGIOGRAPHIC EMBOLIZATION
2. PELVIC PACKING
3. INTERNAL ILIAC ARTERY LIGATION
4. EXTERNAL FIXATION – long bone fracture and open book fracture
5. WOUND DEBRIDEMENT – open wound
EXAMINATION
1. Inability to weight bear
2. Abnormal POSITIONING OF LOWER EXTREMITIES
3. Skin – scrotal, perineal hematoma, perineal laceration, Morel-Lavallee lesion
4. Neurological examination – Lumbar sacral plexus
5. Urogenital examination
6. Vaginal/Rectal examination – to rule out open pelvic fractures
INVESTIGATIONS
EFAST
CT SCAN – from head to toe
Head
Chest
Abdomen
Pelvis
Classification of patients before secondary resuscitation
- STABLE – ETC
- BORDERLINE – DCO
- UNSTABLE – DCO
- EXTREME – DCO
TIMING OF SURGERY
DAY 1
EARLY TOTAL CARE FOR STABLE PATIENTS
DAY 2 – 5
AVOID SURGERY
SIRS
2nd hit is common
DAY 5 – 10
WINDOW OF OPPURTUNITY
AFTER DAY 10
High infection rate
DCO EVOLUTION
1960 s – DELAYED SURGERY
“ too sick to operate on ”
Preliminary traction -> delayed definitive fixation
1980 s – EARLY TOTAL CARE
“ too sick not to operate on ”
ATLS concept plus Advancement in Anaesthesiology and ICU care lead to
– early fixation prevents FES
– early mobilization facilitates nursing care and
– early mobilization prevents pneumonia , sepsis
Patients with ISS > 17 (borderline patients) are at high risk of complications
1990 s – DAMAGE CONTROL ORTHOPEDICS
CONCEPT OF DCO
1. STOP ONGOING DAMAGE
2. STABILIZE LONG BONE
3. STABILIZE PHYSIOLOGY
DCO -> DEFINITIVE STABILIZATION
Multidisciplinary team management :
Orthopedics surgeon
Intensive care specialist
Anesthetist
Nursing care officers
Save life or limb
Control bleeding
Decompression
Decontamination
Splint fractures – cast/traction/EF
EARLY TOTAL CARE: Definitive fracture management within 24 hours
ADVANTAGES :
- Pain relief
- Less infection
- Early mobilization
- Prevent thromboembolism
Constant dynamic approach
?
If physiology deteriorating on table
?
Bail out and switch to DCO
?
Resuscitation in ICU
TARN
TRAUMA AUDIT AND RESEARCH NETWORK
Established in 1990 by THE UNIVERSITY OF MANCHESTER AND LEICESTER
Ultimate goal is improvement in Trauma care
TARN has enabled a system to benchmark practice through monitoring and publishing process measures, allowing on-going and continued appraisal and improvement for the system
Local system -> National system
SCORING SYSTEMS IN TRAUMA
- PHYSIOLOGICAL
- RTS
- APACHE
- SOFA
- SIRS
- ETS
ANATOMICAL
- AIS
- ISS
Anatomical profile
- PATI
- IC-ISS
- TMPM-ICD9
COMBINED
- TRISS
- ASCOT
- ICISS
Purpose of scoring system
1. Appropriate triage and classification of trauma patients
2. Predict outcomes for patients and family counseling
3. Quality assurance
4. As a research tool – extremely useful for the study of outcome
5. Reimbursement purposes
MESS SCORE
Predict the amputation or salvage after lower extremity trauma
1. Skeletal / Soft tissue injury
Low energy – stab/simple fracture/gunshot -1
Medium energy – open/multiple fracture, dislocations -2
High energy – high speed MVA or rifle GSW -3
Very high energy – high speed trauma + contamination -4
2. Limb ischemia
Pulse reduced or absent but normal perfusion -1
Pulseless ; paresthesia , reduced capillary filling -2
Cold , paralysed, insensate, numb -3
3. Shock
SBP > 90 -0
Hypotension transient -1
Persistent hypotension -2
4. Age
< 30 -0 30-50 -1 >50 -2
*** 100% of amputation risk – 7 or more
**100% salvage rate – 4 or less
**DOUBLE the score if ischemia time more than 6 hours
PROS – HIGH SPECIFICITY for predicting amputation
CONS – LOW SENSITIVITY for predicting amputation
REVISED TRAUMA SCORE
WIDELY USED AS PREHOSPITAL FIELD TRIAGE TOOL
In START Triage
3 categories are considered ;
GCS
SBP
RR
Lower score – more severe
< 3 – declared dead / highly unlikely to survive 3-10 – immediately transfer to near trauma center 11 – urgent 12 – delayed care PROS – useful during triage to determine which patients need to be transferred to the trauma centre CONS – can underestimate injury severity in patient injured in one system
INJURY SEVERITY SCORE
It correlates with mortality, morbidity and hospitalization time after trauma
AIS – An anatomically based consensus – derived global severity scoring system that classifies each injury in every body region according to its relative severity on a 6 points ordinal scale.
MINOR – 1
MODERATE – 2
SERIOUS ( LIFE THREATENING ) – 3
SEVERE ( LIFE THREATENING , SURVIVAL PROBABLE ) – 4
CRITICAL ( SURVIVAL UNCERTAIN ) – 5
MAXIMAL ( POSSIBLE FATAL ) – 6
BODY is divided into 9 anatomical regions :
Head
Neck
Face
Chest
Abdomen and pelvic girdle
Spine
Upper extremities
Lower extremities
External
ISS = sum of squares for the highest AIS grades in the 3 most severely injured ISS body regions.
ISS = A2 + B2 + C2
RANGE FROM 1 TO 75
Single score of 6 on any AIS results in automatic ISS of 75
ISS > 15 associated with mortality of 10 %
PROS – integrates anatomical areas of injury in formulating a prediction if outcomes
CONS – difficult to calculate during initial evaluation and resuscitation in emergency room
– difficult to predict outcomes for patients with severe single body area injury
New Injury Severity Score (NISS)
Applied for single body injury area
More predictive of complications and mortality than ISS
Modified Injury Severity Score (MISS)
For children
Anatomical areas are 5 instead of 9
Calculation same as ISS
SIRS
1. HEART RATE > 90/minute
2. WBC count < 4000 cells/mm3 OR > 12000 cells/mm3
3. RR > 20 or PaCO2 < 32 mm
4. TEMPERATURE < 36 degree celsius or > 38 degree celsius
SCORE MEETS 2 OR MORE – SIRS
Leave a Reply