Courtesy: Kshitij Chaudhary, Spine Surgeon, Sir HN Reliance Foundation Hospital, Mumbai
EXAMINATION OF SPINE
1. LOOK
2. FEEL
3. MOVE
4. NEUROLOGICAL
5. SPECIAL TESTS
6. OTHER JOINTS
7. VASCULAR
8. GENERAL EXAMINATION
EQUIPMENTS NEEDED FOR A NEUROLOGICAL EXAM
• Hammer
• 128 Hz tuning fork
• Pen light
• Pins (for testing pain)
• Cotton (for testing light touch)
• Measuring tape
• Tongue depressor
BEFORE YOU START EXAMINING
1. Introduce yourself
2. Confirm patient identity
3. Ask permission
4. Explain what you are going to do
5. Expose the patient- be sensitive
6. BE KIND
1) LOOK
• Gait
• Rhomberg test
• Posture
• Spinal Alignment
• Skin
GAIT
1. Hemiplegic
2. Diplegic
3. Parkinsonian
4. Sensory
5. Ataxic
6. Neuropathic
7. Myopathic
8. Choreiform
HEMIPLEGIC GAIT: The patient stands with unilateral weakness on the affected side, arm flexed, adducted and internally rotated. Leg on same side is in extension with plantar flexion of the foot and toes. When walking, the patient will hold his or her arm to one side and drags his or her affected leg in a semicircle (circumduction) due to weakness of distal muscles (foot drop) and extensor hypertonia in lower limb. This is most commonly seen in stroke. With mild hemiparesis, loss of normal arm swing and slight circumduction may be the only abnormalities.”
DIPLEGIC GAIT: Patients have involvement on both sides with spasticity in lower extremities worse than upper extremities. The patient walks with an abnormally narrow base, dragging both legs and scraping the toes. This gait is seen in bilateral periventricular lesions, such as those seen in cerebral palsy. There is also characteristic extreme tightness of hip adductors which can cause legs to cross the midline referred to as a scissors gait. In countries with adequate medical care, patients with cerebral palsy may have hip adductor release surgery to minimize scissoring.
PARKINSONIAN GAIT: In this gait, the patient will have rigidity and bradykinesia. He or she will be stooped with the head and neck forward, with flexion at the knees. The whole upper extremity is also in flexion with the fingers usually extended. The patient walks with slow little steps known at Marche a petits pas (walk of little steps). Patient may also have difficulty initiating steps. The patient may show an involuntary inclination to take accelerating steps, known as festination. This gait is seen in Parkinson’s disease or any other condition causing parkinsonism, such as side effects from drugs.
SENSORY GAIT:As our feet touch the ground, we receive proprioceptive information to tell us their location. The sensory ataxic gait occurs when there is loss of this proprioceptive input. In an effort to know when the feet land and their location, the patient will slam the foot hard onto the ground in order to sense it. A key to this gait involves its exacerbation when patients cannot see their feet (i.e. in the dark). This gait is also sometimes referred to as a stomping gait since patients may lift their legs very high to hit the ground hard. This gait can be seen in disorders of the dorsal columns (B12 deficiency or tabes dorsalis) or in diseases affecting the peripheral nerves (uncontrolled diabetes). In its severe form, this gait can cause an ataxia that resembles the cerebellar ataxic gait.
ATAXIC (wide based) GAIT
1) Cerebellar gait (tend to sway and stagger to the side of the cerebellar lesion, titubations)
2) Myelopathy / post column dysfunction (Rhomberg positive)
Most commonly seen in cerebellar disease, this gait is described as clumsy, staggering movements with a wide-based gait. While standing still, the patient’s body may swagger back and forth and from side to side, known as titubation. Patients will not be able to walk from heel to toe or in a straight line. The gait of acute alcohol intoxication will resemble the gait of cerebellar disease. Patients with more truncal instability are more likely to have midline cerebellar disease at the vermis.
MYOPATHIC GAIT: Hip girdle muscles are responsible for keeping the pelvis level when walking. If you have weakness on one side, this will lead to a drop in the pelvis on the contralateral side of the pelvis while walking (Trendelenburg sign). With bilateral weakness, you will have dropping of the pelvis on both sides during walking leading to waddling. This gait is seen in patient with myopathies, such as muscular dystrophy.
CHOREIFORM: Not strictly a gait, Writhing movements, Involuntary movements irrespective what they do, Sitting or standing. (Chorea means dancing in unison in Greek)This gait is seen with certain basal ganglia disorders including Sydenham’s chorea, Huntington’s Disease and other forms of chorea, athetosis or dystonia. The patient will display irregular, jerky, involuntary movements in all extremities. Walking may accentuate their baseline movement disorder.
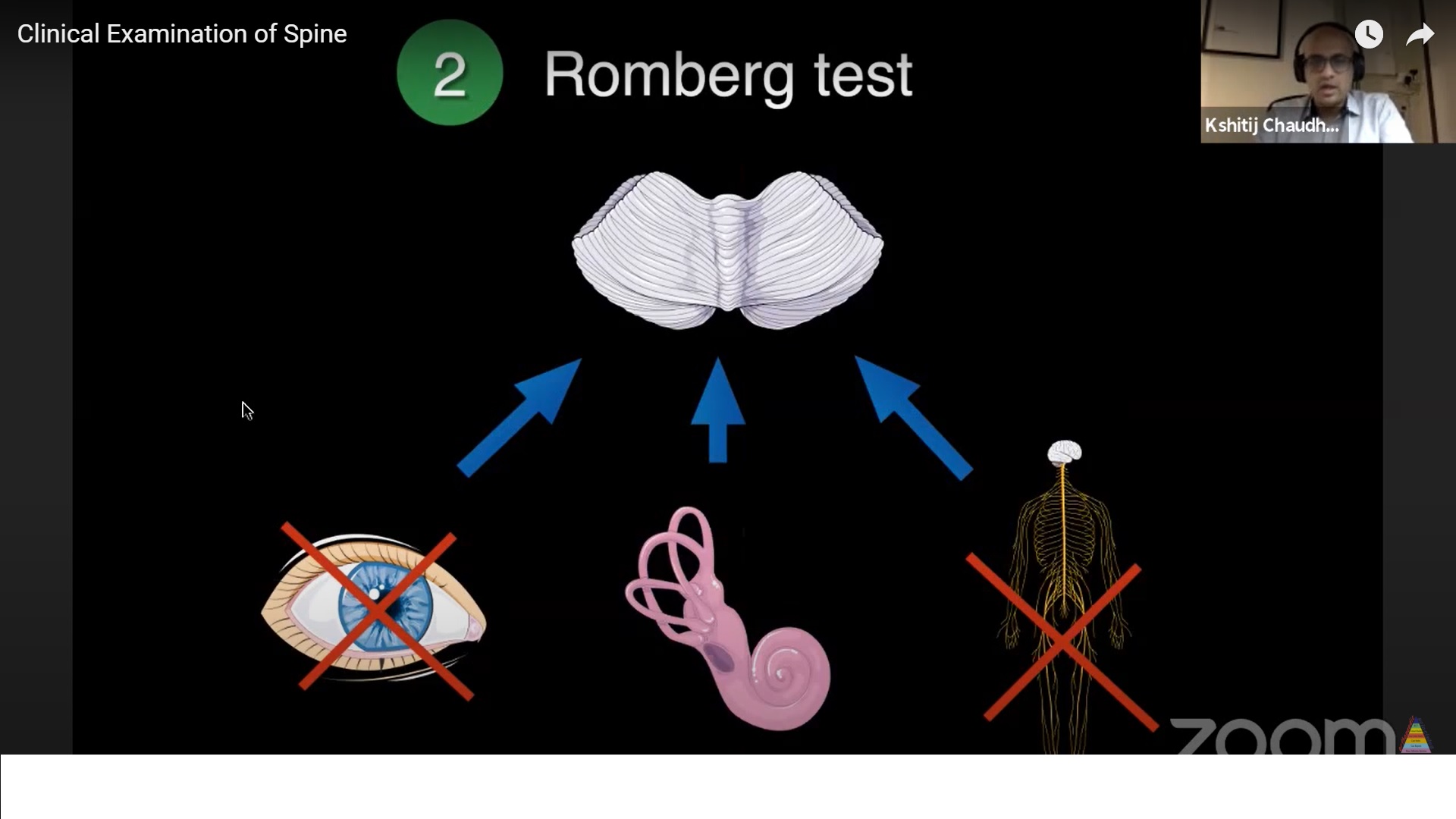
RHOMBERG TEST
*Posterior column dysfunction
*Severe peripheral neuropathy
– Ask the patient to stand with feet close to each other, first with eyes open and then with eyes closed. Be ready to provide support if patient begins to sway and fall. If the patient tends to sway or fall with eyes closed, then the test is considered positive.
This test is not for testing cerebellar dysfunction. To maintain balance, cerebellum uses sensory input from three peripheral systems: vision, vestibular apparatus, and proprioception (joint position sense). Disruption of any one peripheral system can be compensated (completely or partially) by the other two. The test is typically positive in a patient with sensory ataxia due to loss of proprioception (Vit B12 def, diabetic neuropathy, spinal cord compression affecting posterior columns). When the patient closes his/her eyes, visual input is interrupted causing the patient to sway. Cerebellar pathology will cause swaying even with eyes open and this is not considered a positive test.
POSTURE
In erect normal posture
- Head is centered over the pelvis (plumb line)
- In the sagittal profile, the ear, shoulder, greater trochanter and the ankle are in a straight line
- Hips and knees are extended
- Pelvis is horizontal
- Neck is in neutral position and shoulders are at the same level
- Postural abnormalities can be seen in various conditions like kyphosis, scoliosis, degenerative disc disease, spondylolisthesis , torticolis etc.
ALIGNMENT
Coronal plane – straight
Sagittal plane – curve (normal kyphosis and lordosis)
Normal thoracic spine is kyphosis. If decreased – hypo-kyphosis, If reversed – lordosis. If increased – hyperkyphosis
Normal lumbar spine is in lordosis.. If increased- hyperlordosis, lumbar kyphosis is seen in patients with vertebral fractures
SKIN
Look for any swellings or scars or any other abnormal findings
Tuberculosis can present as swelling (cold abscesses)
2.FEEL
1) Local warmth
2) Tenderness (superficial and deep)
3) Bony palpation
4) Soft tissue palpation (muscles, swellings)
3.MOVE
Active range tested
Don’t test in suspected instability / deficit
- Amount of range (accurate measurement are difficult and add little value ,except in AS)
- Whether associated with pain.
- Rhythm (if the motion is halting or with aberrant pattern)
Cervical Spine
* Flexion (80º): Normally, one is able to touch the chin to the chest. Can be quantified by chin-chest distance
* Extension (50º): Normally, one is able to see the ceiling with the forehead almost horizontal. 50% ofFlex-Ex occurs at the O-C1 joint.
*Lateral flexion (45º on either side): Ask patient to try to bring ear as close to shoulder.
* Rotations (80º on either side): Normally, the chin will come close to being above the shoulder. 50%rotations occur at C1-C2 and restriction may indicate C1-2 pathology.
Lumbar Spine(+ Hips)
-Flexion: Normally a person would be able to get the trunk parallel to the floor (flexion of 90º) or get his fingertips within 10 cm off the floor. Wide variation in lumbar flexion among normal individuals. Most of the flexion happens at the hips. To quantify lumbar flexion in isolation, use modified Schober test
-Extension: Ask patient to lean backward. Normal 20-30º.Facet joint arthritis may cause restriction of extension or pain
-Lateral bending: Ask to bend sideways after stabilizing the hip. Assess how far the patient’s hand can travel along the lateral aspect of the thigh towards the knee. Imaginary line from vertebra prominence to the sacrum will normally make an angle of 30º with the vertical. Restricted bending towards the side of the radiculopathy.
-Lateral rotation: Ask patient to rotate spine with the examiner stabilizing the pelvis. Alternatively, perform in sitting position. Usually 30-40º on either side (angle between plane of shoulder and the stabilized pelvis). Most of it is happening at thoracic spine
4.NEUROLOGICAL EXAMINATION
1. Higher mental function
2. Cranial nerves
3. Motor
4. Reflexes
5. Sensory
-Higher mental exam is not needed if patient has given a clear, coherent history.
-Cranial nerves:
Screening: Visual field in one eye, both pupillary response, Eye movements, Facial nerve, Hearing to finger rub
Lower CN (9, 10, 11, 12) involved in CVJ problems.CN 9 and 10 – Say “ahh” tongue depressor, soft palate moves up symmetrically. CN 11 – trapezius and SCM testing.CN 12 – stick patients tongue out(look for deviation).
MOTOR EXAMINATION
1. Inspect ( muscle wasting, fasciculations, atrophy, deformity, contracture)
2. Tone
3. DTR
4. Superficial reflex
5. Power
6. Coordination
Deep tendon reflexes-
• Biceps (C5,C6)
• Supinator( C6,C5)
• Triceps ( C6, C7)
• Knee (L2,L3,L4)
• Ankle(S1,S2)
Note: Inverted supinator reflex- only one response present [brachioradialis(-), biceps(-), finger jerk(+)], lesion at C5-C6
Grading of DTR
0 No response
1+ Reduced or hypoactive
2+ Normal response
3+ Brisk or hyperactive response
4+ Clonus
Note: Absolute reflex grade is heavily dependent of examiner’s interpretation. Symmetry of reflexes (on the left and right) is more important than the absolute reflex grade.
Superficial reflexes-
• Abdominal reflex (T7 to T12)
• Cremastric reflex (L1, L2)
• Anal reflex ( S2,S3, S4)
• Bulbocavernous reflex (S3, S4)
• Plantar reflex( L5, S1)
Power (Lower Extremity)
• Hip flexion L2-L3
• Hip extension L5-S1
• Hip abduction L4-L5
• Knee extension L3-L4
• Ankle dorsiflexion L4-L5
• Plantar flexion S1
Power (Upper Extremity)
• Shoulder abduction C5
• Elbow flexion C5-C6
• Elbow extension C6-C7
• Wrist extension C6-7
• Wrist flexion C7-8
• Finger flexion C8
• Finger extension C7
• Finger abduction T1
Co-ordination
• Upper extremity- finger nose test
• Lower extremity- heel to shin test
SENSORY EXAMINATION
• Pain and temperature fibres cross over at the level of spine, ascend along the spinothalamic tract and reach the sensory cortex
• Posterior column sensations(proprioception and steriognosis) ascend on the same side of spinal cord and decussate at the brain stem the reach the sensory cortex
-RECTAL EXAMINATION(especially in cases of suspected spinal cord injury or cauda equina syndrome)
• Peri anal sensations
• Rectal tone
• Voluntary rectal sphincter contraction
• Anal reflex
5.SPECIAL TESTS
LUMBAR RADICULOPATHY
1. Passive SLR + Forced DF
2. Crossed SLR
3. Femoral stretch test
PSLR and Bragard’stest: Passive SLR reproduces leg pain with L5,S1 radiculopathy.L5 and S1 nerves move 2-6 mm with SLR. In relaxed supine position first test the normal side. Using one hand to ensure knee extension lift the leg passively by holding at the heel. Angle of elevation at which the radicular leg pain is reproduced is measured. If pain is reproduced, lower the leg a few degrees so that there is pain relief. Then passively dorsiflex the ankle to check for reproduction of pain (Bragard’s test)
Interpretation-Test is positive if pain is reproduced between 35 to 70º. In the first 35º the stretch in the sciatic nerve is taken up without translation of nerve roots in the neural foramen. After 70-80º no further translation occurs. The PSLR tests the lower lumbar nerve roots L4, L5 and S1. As sensitivity is high, a positive SLR does not always implicate a disc herniation. However, SLR will be positive in 90% of patients with disc herniation causing radiculopathy. Sensitivity high (80%) and specificity low (40%). Hence, negative PSLR may be diagnostically more important than a positive one
Crossed SLR/ Well legged SLR:Most specific test for disc herniation. Usually indicates an axillary herniation with a free fragment. Pain is reproduced in the involved side on performing a PSLR on the normal side. May indicate a free, extruded fragment. Sensitivity low (30%) and specificity high (88%). Therefore, if CSLR is present then the likelihood of sciatica is high.
Femoral stretch test (L2,3,4):Sensitivity 50%.Specificity 100% . In Prone position, gradually flex the knee completely. If no pain is reproduced, put the hip in extension by passively lifting the thigh off the bed,Reproduction of anterior thigh pain on knee flexion indicates upper lumbar radiculopathy (L2, L3 or L4).
CERVICAL RADICULOPATHY
1. Provocative manuevers
2. Relieving manoeuvres
3. Tests to rule out Peripheral entrapment
Spurling manoeuvre (Provocative): Low sensitivity 50% & High specificity 88%. Stand behind the patient who is seated comfortably. Ask patient to laterally flex the neck on the affected side by 30º.Alternatively, you can ask the patient to both side bend on the same side and look away (rotate on the opposite side).Interlock your fingers and rest your palms over the patient’s head and push downwards without increasing patient’s lateral flexion. Positive if the radiating pain going down the arm is reproduced. Negative test does not rule out radiculopathy
Distraction (Relieving) test: Pain relieving manoeuvre. In order to do this test patient should have cervical radicular pain at rest. High specificity in presence of radiculopathy
Shoulder abduction relief sign: patient is asked to keep arm over the head. Pain reduces by relaxing the brachial plexus
TESTS FOR PERIPHERAL NERVE ROOT ENTRAPMENT
• Phalen’s test
• Tinel’s test
• Durkan’s test
TESTS FOR THORACIC OUTLET SYNDROME
• Adson’s test
• Roos test
• Elevated arm stress test
-MYELOPATHY SIGNS
Hoffman’s reflex- In a relaxed position of hand, middle phalanx of the middle finger is firmly grasped. The terminal phalanx is suddenly flicked down using the examiner’s thumb
Positive response: flexion and adduction of thumb and flexion of index finger. Sometimes other fingers flex as well. Clinical significance controversial. Not pathognomonic of UMN lesion. Not equivalent to “Babinski of the upper extremities”. May be present in healthy individuals (nervous or anxious). Too low positive predictive value (10% for brain lesions to 35% for cervical spine lesions) to be relied as a stand-alone test. Low sensitivity (60%) and specificity (50%) to be relied upon as a screening test for cervical spinal cord lesions
Finger escape sign- Ask patient extend arms with palms facing down and all fingers held together. In Cervical myelopathy – Patient is not able to hold the little finger in adduction for more than 30 seconds. With increasing myelopathy, ring finger and middle finger may show similar tendency and they cannot be held in extension
Finger grip-release test- Ask patient to grip and release fingers as rapidly as possible. Normal person can do this 20 times in 10 seconds. Both finger escape sign and abnormal grip-release are indicative of myelopathy hand.
In ANKYLOSING SPONDYLITIS, in order to quantify the range of motion following measurements are used
1. Cervical mobility- Occiput to wall distance
2. Thoracic mobility- Chest expansion( normal expansion >5cm)
3. Lumbar mobility- Modified Schober’s test(normal > 5cm)
Modified Schober’s test: Accurate measure of lumbar spine motion. Used for monitoring treatment in Ankylosing Spondylitis. 3 marks are made. First, at the lumbosacral junction represented by a line connecting the dimple of Venus on either side. Second, 5 cm below the first line and third, 10 cm above the first line. Keep the measuring tape at the uppermost mark. Make sure that the distance between the uppermost and lowermost markings is 15cm. Ask the patient to touch the toes without bending the knee. Measure the distance between the upper most and lowermost lines. Considered abnormal if does not increase by >5 cm
6.Examination of other joints
1. SI joints
2. Hips
3. Knees
4. Shoulders
FABER (Patrick) test: In supine position keep leg in the figure of 4 position. Stabilize the pelvis at the ASIS using one hand and press down on the ipsilateral knee. Provocative screening test for reproducing pain from the hip, knee, lumbar or SI joint. Cannot be used as a standalone test to rule out sacroiliac pathology as the sensitivity is low (40%).
Gaenslen’s test: Patient is supine at the edge of the bed. He flexes the hip and knee and holds the leg towards chest with both hands. Extend the other leg off the edge of the bed while the other remains flexed. Non tested side is held in hip flexion. Stresses both the sacroiliac joints and pain experienced on the affected side.
7.Vascular system examination
To rule out vascular claudication
Look for varicose veins
Look for cutaneous changes of PVD
8.GENERAL EXAMINATION: do a HEAD TO TOE general examination
Leave a Reply