Courtesy: Prof Nabil Ebraheim, University of Toledo, Ohio, USA
Osteomyelitis is an infection of bone and bone marrow.
What happens in bone infection?
- Usually bacteria causes infection in the bone. Staph aureus is the most common organism in adults.
- Leukocytes are attracted to the area and secrete enzymes in an attempt to kill the bacteria.
- Blood flow to the area is decreased and a devitalized necrotic bone is formed called a sequestrum.
- Sequestrum is a infected dead bone resulting from osteomyelitis.
- Haversian canals surround blood vessels and nerve cells throughout the bone.
- The sequestrum has no connection to the normal bone through haversian system.
- Because of the fact that the sequestrum is avascular (dead piece of bone) antibiotics cannot reach sequestrum or the bacteria.
- In fact the bacteria enters bone cells and hides there.
- Antibiotics alone may not help due to difficulty in penetrating the necrotic area.
- The involcrum is new bone formation around the sequestrum.
- The body tries to seal of the infection by forming new bone.
- The sequestrum drains through the sinus.
- Biopsy of sinus is not representative of the infection. Multiple deep samples preferably bone biopsy and cultures are needed.
- Biopsy of the sinus is important in longstanding cases of osteomyelitis to rule out the formation of squamous cell carcinoma.
Unusual organisms for osteomyelitis:
- Patients with sickle cell anaemia may have osteomyelitis caused by salmonella, however staph aureus is the most common cause.
- Patients with a history of iv drug abuse can have acromioclavicular or sternoclavicular joint infection due to Pseudomonas.
- Patients may also get Pseudomonas from puncture wounds through shoes.
- Immunosuppressed patients and patients on parental nutrition may get fungal osteomyelitis.
Differential Diagnosis of Osteomyelitis
- In children, Eosiniphilic Granuloma, Ewing’s Sarcoma, and Acute Osteomyelitis may resemble each other.
- The patient may have pain, fever, tenderness of the area, and the patient may also have an increased sedimentation rate and leukocytosis.
- Osteomyelitis can also be confused with a benign or malignant tumor.
- Sometimes a biopsy is necessary for the diagnosis.
- Only 50% of chronic musculoskeletal infection will have elevated inflammatory markers.
Classification of Osteomyelitis
Acute – Usually within 2 weeks.
Chronic – After several months
Subacute – From 4 weeks to several months
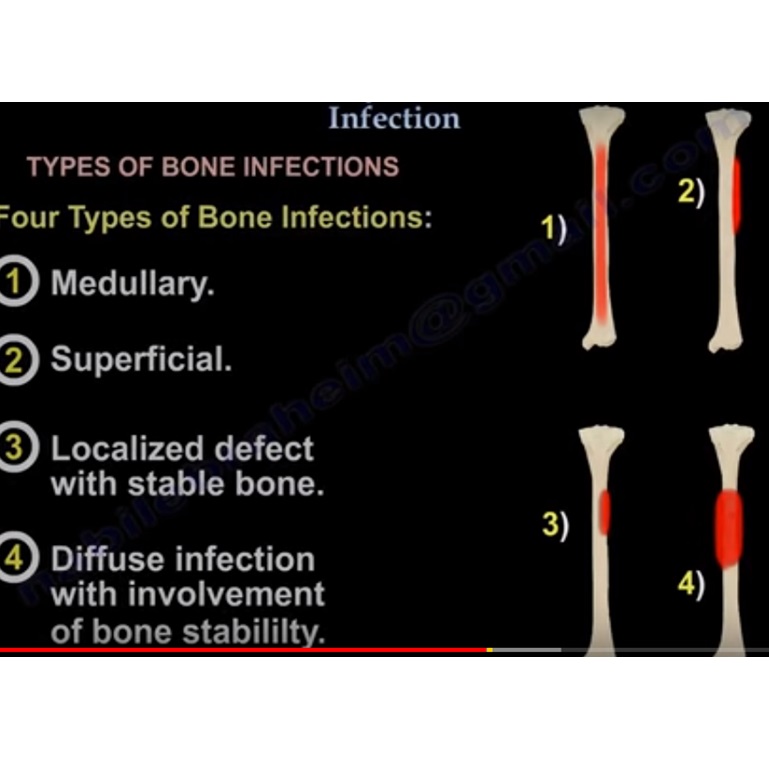
Cierny-Mader Classification System of Osteomyelitis
Three types of patients & Four types of bone infections.
Three types of patients :
A) Healthy
B) Compromised.
*Locally compromised
– Patient had sinus tract, free flap, decreased blood supply.
* Systemically compromised
– patient with medical comorbidities
*Severe systematic compromise
-The host in whom treatment will lead to greater morbidity than the infection itself.
Four types of Bone infections:
1. Medullary.
2. Superficial.
3. Localized infection with stable bone.
4. Diffuse infection with involvement of bone stability.
Principles of surgical treatment for Osteomyelitis:
- Treatment of osteomyelitis is usually a combination of surgical debridement of the necrotic, nonviable tissue plus administration of culture specific antibiotics.
1. Open the involucrum.
2. Remove the Sequestrum (dead bone)
3. Saucerize the bone
-Make sure a pathological fracture is not created.
-Stabilize the bone if needed (external fixator is usually preferred)
4. Fill the cavity with bone chips, cement or muscle flap if needed.
-Intravenous antibiotics are usually given for a period of 6 weeks ( usually organism specific).
-Recurrence of infection is high and occurs in about 30% of cases.
MRSA OSTEOMYELITIS
- Body temperature more than 38 C
- WBC count more than 12,000
- Hematocrit less than 34%
- C-reactive protein more than 13.
These four independent predictors differentiate between MRSA and MSSA osteomyelitis with 92% chance of having MRSA if all the four are present.
- If MRSA is identified, administer vancomycin or clindamycin
- In MRSA, you will have a higher incidence of DVT than other causes of osteomyelitis.
- Older children, 8 years old or more, with MRSA osteomyelitis and CRP more than 6 has a 40% incidence of DVT on presentation.
- The presence of panton – valentine leukocidin(PVL) gene encoded in strains of MRSA bacteria may explain deep venous thrombosis(DVT)
Principles of treatment of Chronic Osteomyelitis
TREATMENT – Careful workup and staging of the bone and the host utilizing the Cierny –Mader classification is important to develop a successful treatment plan.
The principles of treatment of chronic osteomyelitis includes:
- Do debridement first.
- Do dead space management (usually by putting cement spacer with antibiotics).
- Do soft tissue coverage.
- Later on, remove the cement spacer and deal with the bone defect, usually by adding bone graft.
- During this treatment, you can figure out the stability of the bone and add external fixator if needed.
*Masquelet technique (induced membrane):-
- Antibiotic cement spacer followed by the soft tissue coverage, and then do staged bone graft at 6-8 weeks later (induced membrane then later do staged bone graft).
- The membrane secrets Bone Morphogenic Protein 2 (BMP-2) and Vascular endothelial growth factor (VEGF) as well as other growth factors, which peak around 4 weeks after membrane induction.
Leave a Reply