Courtesy: Dr Samir Qureshi, The Young Orthopod Channel
FRACTURE HEALING
Fracture Healing is a specialised type of wound healing consisting of a sequence of inflammation, repair and remodelling that helps to restore an injured bone.
The way a fracture heals depend on the amount of movement occurring between the fracture fragments.
When some amount of movement is present
• Relative stability
• 2 – 10% strain
• Secondary healing via intermediate stages.
When there is no movement (after rigid internal fixation)
• Absolute stability and compression
• < 2 % strain
• Primary healing occurs (direct healing with bone)
Secondary Bone Healing:
A natural way of bone healing especially in tubular bones. Under most circumstances there will be some movement at the fracture site and bone heals with callus formation through five overlapping phases. The five overlapping phases of secondary bone healing includes:
1. Tissue destruction and hematoma formation
Following a fracture, hematoma forms in and around fracture as vessels are torn.
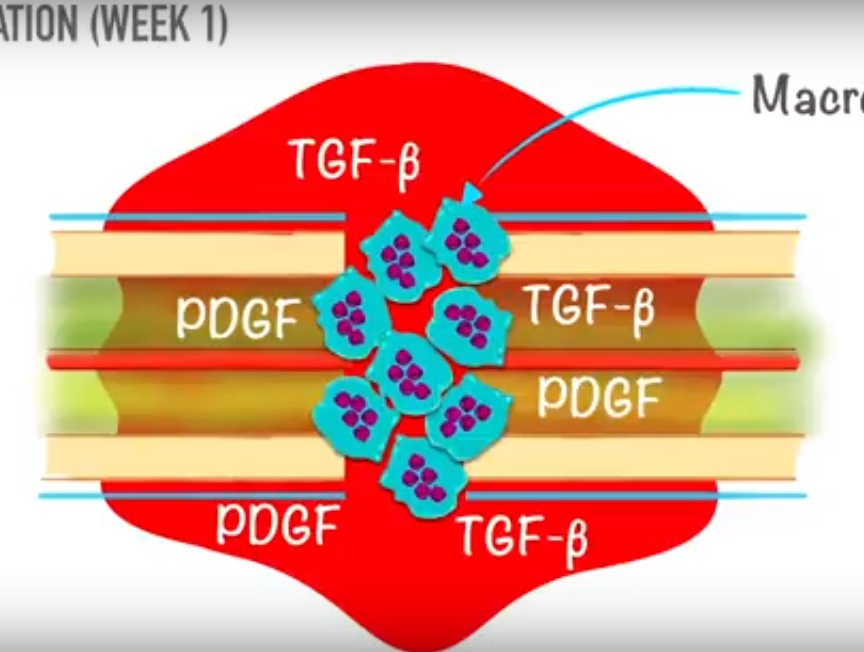
2. Inflammatory phase (week 1)
Within a few hours, an acute inflammatory reaction occurs and the inflammatory mediators like platelet derived growth factor, TGF beta come into play. The clotted hematoma is slowly absorbed and fine new capillaries grow into the area. By the end of this phase the mesenchymal stem cells start to proliferate. These stem cells are derived from periosteum, medullary canal and surrounding muscles.
3. Soft callus formation (week 2-3)
Depending on the local biological and biomechanical environment these stem cells differentiate into fibroblast, chondroblast and osteoblast. Simultaneously, the osteoclasts clear up the dead bone. The granulation tissue is gradually replaced with cartilage and fibrous connective tissue.
The thick cellular mass with its islands of immature bone and cartilage forms the callus or splint on the periosteum and endosteal surfaces. The fracture ends become sticky and movements are reduced. Bone formation begins within the soft callus where the strain is lowest.
4. Hard callus formation (week 4-12)
Bone can be formed in two ways a) endochondral ossification and b) intramembranous ossification. Calcium is laid down in the matrix and the callus then becomes visible on radiograph. As the immature fibre bone or woven bone becomes more densely mineralized, movement and strain at fracture site decreases progressively. With continuing osteoblastic and osteoclastic activity, the woven bone is transformed into lamellar bone. Osteoclasts clean up the debris and osteoblasts fill the gap with new bone. The fracture has consolidated once it has completely healed with the bridging bone.
5. Remodelling of bone (months to years)
Now the fracture has been bridged by a cuff of solid bone, over a period of months or years the crude weld is reshaped by a continuous process of alternating bone resorption and formation. This is the same process that occurs in routine skeletal turn over as well as in primary bone healing.
Primary Bone Healing:
This is seen following internal fixation and compression where the fracture is reduced and held with absolute rigidity. Also, similar pattern of healing seen in impacted fracture in cancellous bones.
Two patterns of primary bone healing are observed
1. The Gap Healing
New capillaries and osteoprogenitor cells growing in from fracture edges fill the gap and new bone is laid down on the exposed surface. In conditions where there is a very narrow gap, directly Lamellar bone is formed.
For wider gaps, initially woven bone which is then remodelled to lamellar bone.
2. Contact healing
When fracture surfaces are in intimate contact and held rigidly from the outset, internal bridging may occasionally occur without any intermediate stages.
In primary healing by 3 – 4 weeks, bone remodelling units start acting, which then organises lamellar bone to create a brand new haversian system.
very useful video for refreshing the minute details, nice presentation.