https://www.youtube.com/live/qXqz7foVUA4?si=s2ltdgempNzhFs8h
Lateral condyle of humerus fracture
Classification of the Lateral Condyle Fracture
- Milch – morphology
- Weiss – displacement
- Song – displacement and stability
Milch Type 1
• Fracture exits LATERAL to trochlear groove
Stable
Milch Type 2
• Fracture exits MEDIALLY into trochlear groove
• Unstable
Milch – modified
• Uses the capitello-trochlear sulcus as landmark
Milch classification is less reliable. doesn’t say about treatment outcome and what treatment to follow
Weiss
• Built on Jakobs Classification
• Displacement
• Articular integrity
| Weiss Classification
Type |
Displacement |
Articular Surface |
| I | < 2mm | Intact |
| ll | > 2mm < 4mm | Intact |
| III | > 4mm | Disrupted |
Weiss classification treatment plan
- Weiss type l : Casting
- Weiss type ll : Closed reduction + fixation
- Weiss type lll : Open reduction + fixation
| Song Classification
Stage |
displacement |
fracture |
stability |
| 1 | <2mm | Metaphysis only
Minimal gap |
stable |
| 2 | <2mm | Lateral gap only | Unknown |
| 3 | <2mm | Gap complete | Unstable |
| 4 | >2mm | Without rotation | Unstable |
| 5 | >2mm | With rotation | Unstable |
Song stage 1 and 2 : Cast
Song stage 3 : Closed reduction and fixation
Song stage 4& 5 : open reduction and fixation
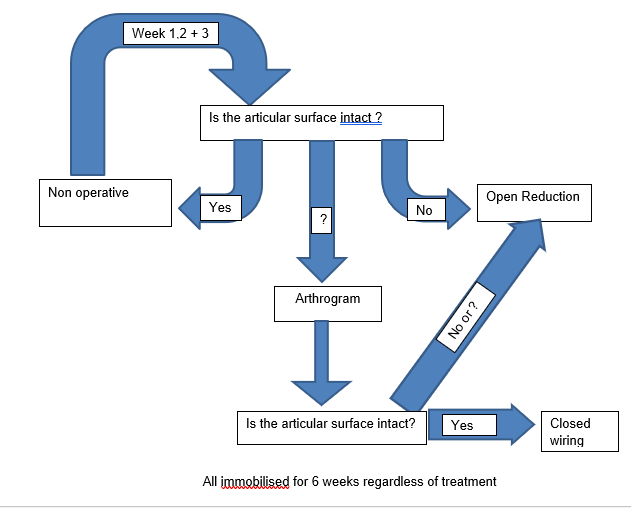
How to treat Lateral condyle fracture?
Accuracy of radiograph : it underestimates displacement by 1.6 – 6.0mm
Metaphyseal Plastic Deformation
• Fragment has changed shape
1) Articular surface displacement is key
2) Radiographs can’t accurately demonstrate this
3) Metaphyseal displacement is not a surrogate for articular displacement or reduction
All immobilized for 6 weeks regardless of treatment
Non operative management
• Undisplaced fractures’ subsequently ‘displace’ frequently (up to 15%)*
• So give yourself the best chance of picking this up
Active non operative management
• AP, lateral and internal oblique Xrays Out of plaster should be obtained at 1, 2 and 3 weeks post injury
• If acceptable, total 6 weeks in plaster
Open reduction and screw fixation
- For large metaphyseal fragment
- Stay outside of growth plate
- Stable internal fixation
- More posterior than posterolateral……
- Good approach if there is a reasonable metaphyseal fragment
- Small fragment bone clamp in olecranon fossa
- 2.7mm cortical screws work well – ? Washers
- Ensure screw engages far cortex!
- If there’s a problem – revise promptly
Late presentations- Non-union lateral condyle humerus
- Late presentations are not uncommon in our country
- Diagnosis is difficult, functional loss of motion is not so severe, financial constraints, native bone setters
- Late presentations or non unions- when there is no attempt of callus or fracture line clearly visible after 2-3 months
- There are clear guidelines for late presenting lateral condyle non unions
- Fontanette- open reduction should not be done 3-4 weeks after injury’
- Wilkins- ” If we believe fracture union can be obtained without loss of motion and avoidance of AVN of lateral condyle, then we recommend surgery for selected patients”
- Open reduction- difficulty in distinguishing the metaphyseal and articular region of fragment, overgrowth of condylar fragment, fibrosis, contracted soft tissues
- Elbow stiffness and avascular necrosis can ensue
- In situ or percutaneous screw fixation- safe and minimally invasive minimal risks of elbow stiffness, blood supply disruption
1) Percutaneous screw fixation promotes Healing of lateral condyle nonunion in children
(J Pediate orthop 2014:34:155 -160)
- 16 patients in age group 2-10
- 12/16 (75% united after surgery- mean of 15.7 wks from injury
- 4/16 (25%) failed to unite- mean of 225 weeks from injury
- Technique successful if non union addressed within 16 weeks from injury
- Minimally invasive with no risks of complications encountered with open reduction
Treatment modality for late presenting non unions- lack of consensus: In-situ fixation, open reduction and bone grafting; corrective osteotomy with or without ulnar nerve transposition
- Moving from era of neglect to era of intervention
- Reduce deformity and instability by trying to restore anatomy In situ / open reduction/corrective osteotomy
- Discuss pros and cons with patient and parents- informed decision on a case by case basis
Take Home
- Lateral condylar fracture of humerus in children have significant long term sequelae
- Late presentations challenging . Assess carefully the clinical problems
Post op radiographs
- Keep watch on ‘funny looking’ post surgery radiographs
When in Doubt
- Oblique, varus stress films
- Contralateral radiographs
- Arthrogram
Leave a Reply