Courtesy: Prof Nabile Ebraheim, University of Toledo, Ohio, USA
Maisonneuve Fractures of the Ankle
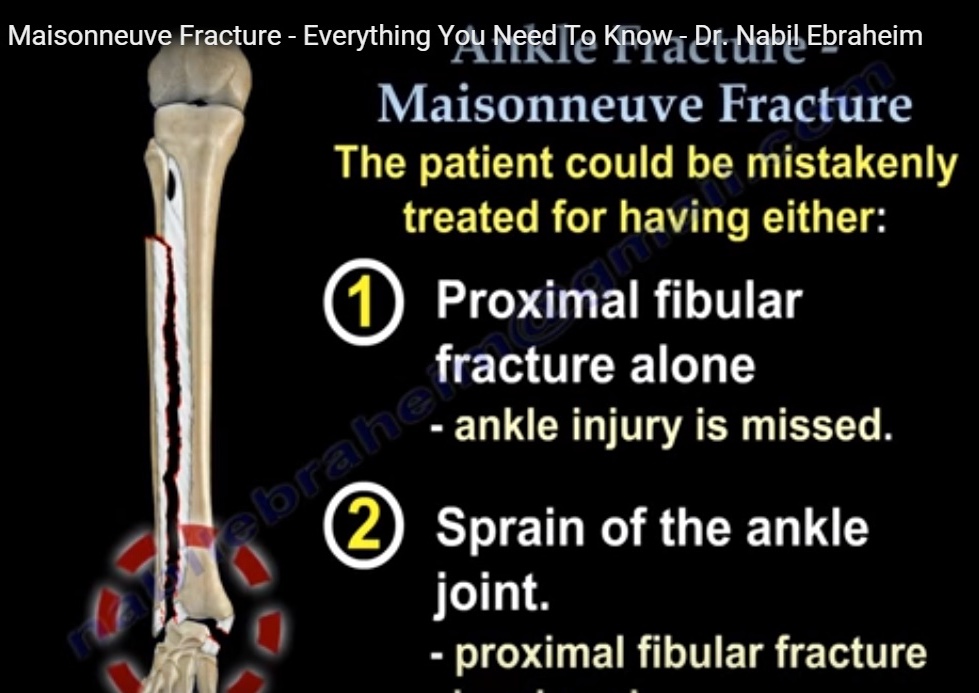
• It is high fracture of the fibula caused by an external rotation mechanism,
• often associated with injury to the tibiofibular syndesmosis.
• Jules Maisonneuve (1840) initially described a “subcapital fracture of the fibula” associated with rupture of the anterior tibiofibular ligament (ATFL)
“Maisonneuve-like” fractures: fibula remains intact but there is injury to the tibiofibular joint, with or without dislocation of the fibular head at the proximal tibiofibular joint
Current Definition:
• An MF is best defined as a fracture of the proximal quarter of the fibula.
• It is combined with at least:
- Rupture of the anterior tibiofibular ligament (ATFL).
- Rupture of the interosseous tibiofibular ligament
History
- First described in 1840 by French surgeon Jules Germain François Maisonneuve.
- The term “Maisonneuve fracture” (MF) became widely known through the work of surgeons Quenu, Chaput, and Destot
- 1966: Weber categorized MFs as unstable injuries, with the interosseous membrane torn up to the level of the fibular fracture.
- 1976: A landmark study by Pankovich provided significant insights into MFs.
- 1981: Ammann published one of the first series of surgically treated MF cases.
- 2019: Bartoní?ek et al. detailed the pathoanatomy of 54 MFs, supported by 3D CT reconstructions.
Epidemiology
• Incidence: 3.5% to 7.0% of all ankle fractures.
• Bilateral Occurrence: rare
• Gender Distribution:
• Male-to-female ratio varies,
• males are more commonly affected.
• Age Distribution: mean age typically 48 years (range: 19 to 78 years).
• Peak age – fifth decade for men and the sixth decade for women
Mechanism of Injury
Primary Cause:
• External rotation injury, typically resulting from high-energy trauma.
• Detailed staging described by Pankovich
Other mechanism
•Most frequently occurs through a pronation-external rotation force, as classified by Lauge-Hansen.
•Rare cases involve a supination-external rotation mechanism with plantarflexion
Pankovich’s Classification
1. Rupture of the anterior tibiofibular ligament (ATFL) or avulsion fracture, often paired with rupture of the interosseous tibiofibular ligament (IOM).
2. Fracture of the posterior tibial tubercle or rupture of the posterior tibiofibular ligament (PTFL).
3. Rupture of the anteromedial joint capsule or avulsion fracture at its insertions.
4. Fracture of the proximal fibula (subcapital fracture).
5. Rupture of the deltoid ligament or fracture of the medial malleolus
Clinical Examination
• Pain and swelling in the malleolar region.
• Crucial to palpate the entire length of the fibula, including:
• Anterior and posterior aspects of the distal tibia.
• The malleoli to assess for fractures or instability
• Tibiofibular Squeeze Test: Compression of the fibula against the tibia.
• Helps identify injury to the tibiofibular syndesmosis.
• External Rotation Test: Applying external rotation to the foot against a fixed lower leg.
• Can point to syndesmotic injury.
• Fibular Head Stability Test: Checking the stability of the fibular head in the proximal tibiofibular joint.
• A positive finding suggests injury to the interosseous membrane (IOM) and syndesmosis.
Imaging
Basic Radiographic Examination:
• Initial radiographs should include anteroposterior, mortise, and lateral views of the ankle.
• For suspected Maisonneuve fractures, anteroposterior and lateral radiographs of the entire lower leg should be obtained.
• Bartoní?ek et al. found that a fracture of the proximal fibula was not visible in 24% of cases on the anteroposterior view.
Stress Radiographs:
• External rotation stress radiographs (using a handheld device) may help reveal latent diastasis in rare cases of nondisplaced MF.
• Pathological widening: A tibiofibular and/or medial clear space of >2mm is considered pathological.
CT Imaging
• Done in suspected or diagnosed through radiographs.
• CT provides detailed information on:
• Position of the distal fibula in the fibular notch.
• Displacement of posterior malleolus fractures.
• Fractures of the Chaput-Tillaux tubercle (CTT), often missed on radiographs.
• Compression of the lateral tibial plafond or osteochondral fractures of the talus.
• Weight-bearing CT can detect subtle syndesmotic injuries with high intra- and interobserver agreement.
MRI:
MRI provides detailed information
• on the degree of ligament injury
• does not assess instability.
• Not typically indicated for acute MFs
• useful in cases with unclear injury patterns or additional cartilage injuries.
Arthroscopy:
• Arthroscopy allows excellent diagnosis of syndesmotic instability and intra-articular injuries.
• It should be considered with caution due to its invasive nature, costs, and risks.
Pathoanatomy
- Complex and Variable Pathoanatomy:
• Recent CT studies show that MF pathoanatomy is more complex and variable than initially described. - Injury to the Proximal Aspect of the Fibula:
• fractures in the subcapital region or the proximal quarter.
• Fractures are usually spiral, and comminuted fractures are rare.
• A rare variant: A 2-level fibula fracture (both proximal and distal) is known as a “double MF” — only 14 cases have been reported. - Injury to the Tibiofibular Syndesmosis & IOM:
• ATFL rupture and interosseous tibiofibular ligament (IOM) rupture are always present in MF.
• IOM rupture is generally limited to the distal third of the IOM (up to 112mm above the ankle joint).
• Recent studies question the necessity of IOM rupture extending all the way to the level of the fibular fracture. - Injury to Medial Structures:
• Injuries to the medial malleolus (MM), deltoid ligament (DL), or both are common.
• MM fractures occur in 39% of cases, and DL ruptures are seen in 51%.
• Fracture patterns in MM: Anterior colliculus fractures are seen in 19%, and bi-collicular fractures are present in 56%. - Fractures of the Posterior Malleolus (PM):
• PM fractures occur in 77% to 83% cases, > general ankle fractures.
• Common fracture patterns: Type-2 (posterolateral) fractures are seen in 50% of cases. - Fractures of the Anterior Malleolus (CTT):
• CTT fractures occur in 17% of MF cases, often with anterolateral tibial plafond compression. - Injuries to Lateral Collateral Ligaments:
• Ruptures of the anterior talofibular ligament (ATFL),
• calcaneofibular ligament,
• posterior talofibular ligament (PTFL)
• These findings suggest a supination injury in certain cases. - Fibulotalar Relationship:
• Proximal shift of the fibula and disruption of the Weber indices are indicative of high fibular fractures, including MFs.
• The lateral gutter between the fibula and talus remains congruent in most MF cases. - Osteochondral Fractures of the Talus:
• Occurs in about 7 cases of MF.
• Lesions are predominantly medial, with one case showing a lateral lesion.
Principles of Treatment for Maisonneuve Fracture
General Treatment Approach:
• MF is considered an unstable injury, and surgical treatment is the standard.
• Nonoperative treatment is rarely indicated, only for undisplaced fractures without latent diastasis.
• Diagnosis of syndesmotic instability is critical and may require fluoroscopic stress testing, weight-bearing CT, or arthroscopy.
Fracture of the Fibula and Its Malpositioning in the FN
• Main goal: Anatomic reduction of the distal fibula into the fibular notch (FN).
• Correct misalignment:
• External rotation.
• Sagittal displacement.
• Shortening of the fibula by ?2 mm.
• Lateral shift and valgus tilt of the talus.
• Internal fixation of the proximal fibular fracture is typically not required and carries a risk of common peroneal nerve injury
Medial Malleolar (MM) Fracture:
• Displaced MM fractures should be reduced and fixed.
• For bicollicular MM fractures, reduction and fixation help maintain the position of the talar dome and medial stability.
• Fixation of AC with only anterior deltoid ligament (DL) attachment does not affect medial ligament stability.
Rupture of the Deltoid Ligament (DL):
• DL repair is not mandatory if the medial clear space is normal after fibular fixation.
• Open revision may be needed if ligament interposition prevents reduction or if there is gross medial instability.
• DL repair may be beneficial in cases with syndesmotic instability to reinforce syndesmotic repair.
Fracture of the Posterior Malleolus (PM):
• Reduction and fixation of PM fractures may restore:
• Tibiotalar congruity.
• Stability of the tibiofibular mortise.
• Integrity of the fibular notch.
• Type-4 (triangular) and displaced or impacted type-2 and type-3 PM fractures should be anatomically reduced and stabilized.
Rupture or Avulsion of the Anterior Talofibular Ligament (ATFL):
• No evidence for direct suturing of the ATFL, although sutures may be added during open reduction of the distal fibula.
• For larger avulsion fractures involving the fibular notch, reduction and fixation are necessary to restore:
• FN integrity.
• Joint congruity.
• Mortise stability.
Surgical Technique for Maisonneuve Fracture
Sequence of Reduction and Fixation:
• Anatomic reduction of the distal fibula into the fibular notch (FN) is the primary goal.
• If present, PM fractures (type-2, -3, or -4) should be reduced and fixed first to restore FN integrity.
• MM fractures (especially bicollicular) should be reduced to help maintain tibiotalar alignment.
• Avulsions/fractures of the CTT are typically reduced and fixed last after tibiofibular stabilization.
Approaches and Patient Positioning:
• Anterolateral Approach for open reduction of the distal fibula.
• Supine position for standard cases.
• Prone position for displaced PM fractures with a posterolateral approach (higher reduction and fixation success).
• Posteromedial approach for Barton?cek-Rammelt type-3 PM fractures; can be done with patient in prone or lateral decubitus position.
• Medial approach for MM or DL repair, depending on patient position
Techniques of Reduction and Fixation of Distal Fibula:
• Dissect crural fascia, deflect the ruptured ATFL for inspection of the 3-corners region (CTT, Wagstaffe tubercle, talar dome).
• Reduction techniques:
• Use curved bone forceps along the transmalleolar line.
• Anteroposterior reduction achieved with bone hook or manual pressure.
• External rotation correction with bone clamp or Kirschner wire as a joystick.
• Once the reduction is adequate, temporarily fix with Kirschner wire.
• Ensure lateral tibiotalar alignment and palpate the anterior tubercle of the fibula and tibia.
Fixation Methods:
• Two transsyndesmotic screws (3.5 mm recommended) are commonly used for stabilization.
• Alternatives: Flexible suture-button implants may offer equal or superior functional outcomes.
• Screw placement:
• Ensure placement 1-4 cm above the tibial plafond.
• The distal implant is inserted first to prevent malpositioning.
Postoperative Care:
• Short leg cast/splint for wound healing.
• Protected weight-bearing for 6-8 weeks using a boot or cast.
• Screw removal:
• 6 to 8 weeks post-op: typically recommended for symptomatic cases or complications.
• Longer removal time (3-9 months) may reduce risks of secondary diastasis.
• Postoperative radiographs to monitor reduction and assess for complications.
Outcomes of Surgical Treatment
Study Results:
• In studies with >10 patients, surgical outcomes for MF treatment have been reported as excellent or good in 80% to 88% of patients.
• Variability in evaluation methods:
• Different outcome scores were used across studies.
• Details on fibular reduction (open vs. closed) and PM fracture fixation were often not mentioned.
• Pre/postoperative CT imaging was not utilized in many studies.
Key Prognostic Factor:
• Anatomic reduction of the distal fibula into the FN is the most important factor in predicting successful outcomes.
• Larger studies, particularly those that incorporate CT-based analysis and validated outcome measures, are needed to define more specific prognostic factors for MFs.
Common Features of MFs:
• Typically involve ATFL lesions and high fibular fractures.
• Often associated with other fractures, such as posterior or anterior distal tibial avulsions (detected via CT).
Conclusion
• Open reduction of the tibiofibular syndesmosis is strongly recommended under direct visualization.
• Postoperative CT imaging may be necessary to confirm reduction and ensure favorable alignment.
• Achieving anatomic reduction of the distal fibula within the FN remains the most important prognostic factor for achieving good functional outcomes.
It was very important information
Thanks