Clinical Examination of Lower Limb Deformity
Rajesh Purushothaman, Associate Professor, Medical College, Kozhikode, India
- When a child is born, it has 10-15 degrees of physiological genu varum, 5 degree internal tibial torsion and external rotation contracture of the hip. It reaches the maximum by about 9-12 months. This usually gets corrected to neutral by the age of 18-24 months then the limb develops a valgus angulation, which reaches the maximum of about 12 degrees by the age of 3-4 years. This physiologic valgus usually gets corrected to the adult value of 7 degrees of valgus by the age of 8 years. Physiologic valgus is bilateral and symmetrical; less than 15 degrees and the inter-malleolar distance doesn’t exceed 8 centimetres.
- Tibial torsion is the angle between the transverse axis of the knee and the transmalleolar axis. The tibia is internally rotated at birth. Internal tibial torsion is 5 degrees at birth and gets corrected to neutral by 4-5 years of age. The tibia then gradually becomes externally rotated and reach the adult value of 20-25 degrees of external rotation by the age of 8 years.
- Femoral anteversion is the angle between the transcondylar axis and the longitudinal axis of the femoral neck in the horizontal plane. Femoral anteversion is 40 degrees at birth and reaches the adult value of less than 15 degrees by the age of 8 years. It produces intoeing gait which gradually increases during the first five years of life due to summation of deformities. It gets corrected by 8 years of age.
- Deformity is defined as a deviation from normal structure or function which may be symptomatic or has the potential to produce symptoms.
Goals of deformity assessment
The goal of deformity assessment is to answer the following questions.
1. Is there a deformity?
One should be able to differentiate between physiological and pathologic malalignment.
2. What is the deformity?
Identify the name of the deformity.
3. Where is the deformity?
Identify the site of deformity whether it is at the joint level or in the bone. If in the bone, then it is in the epiphysis, metaphysis or diaphysis. Deformities due to tilting of the joint line becomes less when the joint is flexed. This is because the area of contact between the articular surfaces is altered during flexion.
4. Which is the plane of deformity?
Identify the alteration produced by the deformity in all three planes and any associated limb length discrepancy as well. Thus a deformity may have a component of flexion or extension in the sagittal plane, varus or valgus in the coronal plane, internal or external rotation in the axial plane; in addition there may be shortening or lengthening as well.
5. How severe is the deformity?
Identify the severity of deformity in each plane and also the severity of limb length discrepancy. Assess how much of passive correction of the deformity is possible.
6. Why there is a deformity?
Identify the cause of deformity. Identify whether it is a localised problem or part of a systemic disease. Try to detect whether it is due to soft tissue contracture, muscle paralysis or spasm or rupture, joint dislocation or subluxation or malformation and lastly bony malunion or nonunion or deformation.
7. Are there any consequences of the deformity?
Identify whether there are any compensatory malposition of neighbouring joints and secondary effects such as osteoarthritis on the concave side or laxity of ligaments on the convex side. Assess whether it is associated with any secondary joint instability such as patellofemoral instability in genu valgum. Identify how it is affecting the gait or joint function.
8. When does the deformity occur?
Identify whether it is a static or dynamic deformity.
History
From the history try to understand the relevant details about the deformity, look hints that help identify the cause and understand the secondary effects of the deformity and its impact on function. History should start with the following questions.
• How long the deformity is present?
• How did it start?
• How is it progressing?
• Any associated symptoms?
• Is there any history of trauma or infection?
In children get perinatal history
• Did the mother take any drugs during pregnancy especially in the first trimester?
• Did the mother have any infections especially in the first trimester?
• Did the mother have any history of substance abuse?
• Is there any maternal health problems?
• Did prenatal ultrasounds show any abnormality?
• Was there any abnormality in previous pregnancies?
Get a natal history in appropriate case.
• Was it a full term delivery?
• What was the type of delivery?
• What was the type of presentation at birth?
• What was the birth weight?
• Was there any delay in first cry?
• Were there any complications during delivery?
Get details of nutrition to assess the chance of nutritional deficiencies like rickets.
• Vegetarian or non-vegetarian
• Calorie intake
• Food fads
• Exposure to sunlight
• Whether diet is balanced or not
Family history
• H/o similar or other deformities
Developmental history
• When did social smile appear?
• When did the child achieve
• Neck steadiness
• Sitting
• Standing
• Crawling
• Walking
• Stair climbing and descending
• Hand to hand transfer
General Examination
In general examination look for features of generalised ligamentous laxity, general manifestations of rickets or known dysplasias.
Inspection
Inspect the patient in standing, sitting, walking and in the supine position. Inspect from the front, back and both sides. Look for any asymmetry in size, shape and function.
Look at
• Head tilt and rotation
• Level of shoulders, scapula and iliac crests
• Look for spinal deformity such as scoliosis or kyphosis
• Look for lumbar lordosis suggestive of flexion deformity of hip when the patient is supine on a hard surface
• Look for knee deformity in all three planes
• Look for ankle equinus or calcaneus deformity from the side
• Look for any hindfoot varus or valgus from the back
• Look for any forefoot or toe deformity
Palpation
Palpate the bone, soft tissues and joint. Look for change in temperature; limb with post-polio residual contracture is cold. Look for any tenderness and note the site of tenderness. When palpating bony and soft tissues; look for any asymmetry, thickening, swelling or defect.
Movements
Assess the active and passive movements of spine, hip, knee and the foot and ankle. Record the range of movement. Look for restriction of range of movement, pain during joint movement, ligamentous laxity, joint instability and any abnormal sounds during joint movement. While moving the joint passively, watch out for muscle spasm. Movement should be assessed in all three planes depending on the normal movement for that particular joint.
Measurements
Measurement is done to detect any limb length discrepancy, to assess degree of muscle wasting. Limb length discrepancy may be true or functional. True LLD is due to real shortening or lengthening. Functional LLD is due to abnormal joint positioning such as adduction contracture of hip. Girth of the thigh is measured 15 cm above the knee joint line and girth of the calf is measured at the bulkiest area.
In addition measure intercondylar distance between medial femoral condyles in the standing position for genu varum. In cases of genu valgum measure the intermalleolar distance in the standing position.
Torsional profile of the lower limb
- Torsional abnormalities may be in the femur, tibia or foot. Torsional abnormalities lead to either in-toeing or out-toeing. Intoeing is more common. Commonest cause of intoeing in children below one year is metatarsus adductus, commonest cause from 1-3 years is internal tibial torsion; and after 3 years of age excessive femoral anteversion is the commonest cause. It is identified by assessment of foot progression angle. Foot progression angle is the angular difference between the direction of walking and the long axis of the foot. If the foot is externally rotated then the angle is positive and if internally rotated then the angle is negative. Normal value for children and adolescents is 10 degrees.
- Femoral anteversion is assessed by doing the Craig’s test. It is done in the following method.
Patient position – Prone
Joint position – Knee flexed to 90 degrees.
Procedure- One hand of the examiner is placed flat on the greater trochanter. Hold the leg and gently rotate the hip in both directions till the greater trochanter is maximally prominent. The amount of internal rotation needed to make the greater trochanter maximally prominent is the degree of anteversion.
In addition the range of rotational movement of the hip is also recorded. The patient is made prone and the pelvis is made level. Then rotate the hip internally and externally to the maximum point to which it is maintained by gravity alone. In patients with excessive femoral anteversion, the range of internal rotation is increased and external rotation is diminished. In femoral retroversion, the external rotation is increased and internal rotation diminished.
Tibial torsion is assessed by the thigh foot angle or angle of the transmalleolar axis.
- Thigh foot angle is assessed by the following method.
Patient position – Prone
Joint position – Knee flexed to 90 degrees, ankle in neutral position.
Procedure – Measure the angle between the thigh axis and the foot axis. Angle is negative if internally rotated and positive if externally rotated. Normally the angle is 10 degrees in adults. In the newborn, there is 5 degrees internal tibial torsion normally.
If the foot is not normal, then measure the angle of the transmalleolar axis.
Patient position – The patient is asked lie prone on a couch with the knee flexed to 90 degrees.
Procedure – The centre of each malleoli are marked. Connect these points by a line across the plantar surface of the sole. Draw a line perpendicular to it.
Interpretation – The angle between the thigh axis and a line perpendicular to the transmalleolar axis is measured, which is equal to the tibial torsion.
- Torsional deformity of the foot is assessed by heel bisector line. Heel bisector line divides the heel into two equal halves in the longitudinal axis. In the normal foot it passes through the second toe. If it passes medial to the second toe, forefoot is abducted and if it passes lateral to the second toe, the forefoot is adducted. If it passes through the third metatarsal, adduction deformity is mild, through fourth metatarsal is considered moderate and through fifth metatarsal is considered to be severe metatarsus adductus.
In newborn feet, V- finger test is done to assess the forefoot adduction. The heel of the child is placed in the second interdigital cleft of the examiner. Normally the lateral border of foot is straight and will be in contact with the examiners finger. If the lateral border of the foot beyond the fifth metatarsal base is not in contact with the examiner’s finger due to medial deviation, then there is metatarsus adductus deformity.
Angular profile of the lower limb
- Angular deformities may be physiological or pathological. It is more likely to be pathological if it is unilateral; asymmetrical; painful or if progressive.
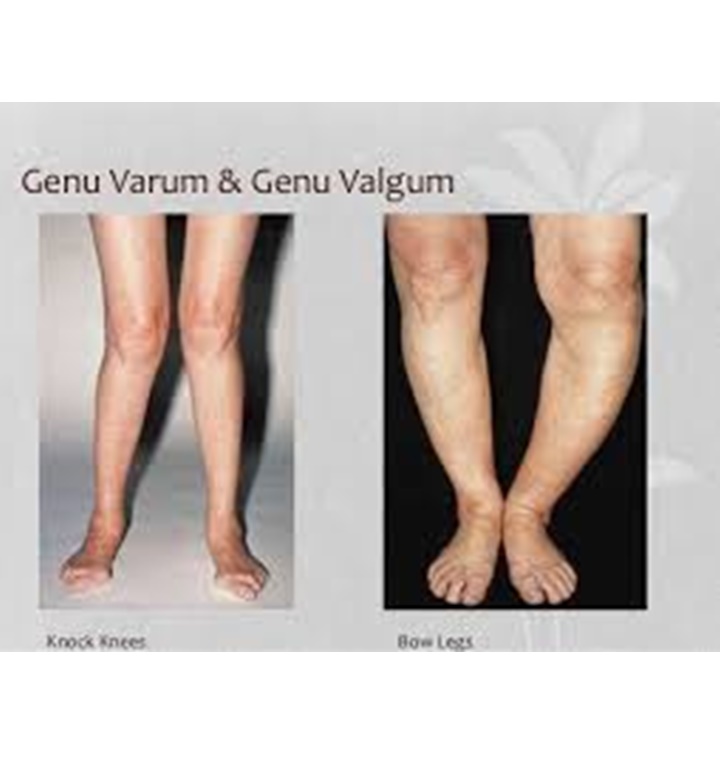
- Ask the patient to stand with his feet and knee touching each other while the patella is facing forwards. When inspected from the front, there will be a gap between the knees in patients with genu varum. In patients with genu valgum, the ankles will be kept apart. Inspect from the side, specifically looking for equinus or calcaneus deformity of ankle, flexion deformity or hyperextension deformity of knee.
- Ask the patient to lie supine on a hard couch and look for any lumbar lordosis suggestive of fixed flexion contracture of hip. If present do the Thomas test to assess the severity of flexion deformity.
Thomas well leg raising test
Patient position- Supine
Examiner position – Stand on the right side of the patient with one hand under the lumbar spine of the patient. With the other hand hold the unaffected side.
Procedure- Flex the unaffected knee fully, then flex the unaffected hip till the excessive lumbar lordosis disappears. Measure the angle between the thigh of the affected side and the couch to assess the angle of fixed flexion deformity of the hip.
Intercondylar distance is measured to assess the severity of genu varum deformity. Ask the patient to stand with his medial malleoli touching each other and then measure the distance between the medial femoral condyles. Intermalleolar distance is measured in patients with genu valgum deformity. Ask the patient to stand with his medial femoral condyles touching each other and the foot should be in neutral rotation, measure the distance between the medial malleoli. Both these measurements have the disadvantage of being influenced by the size of the patient. In this situation, measurement of the tibiofemoral angle using a goniometer is essential. This is measured in the standing position. Lateral thigh leg angle is measured by keeping the arms of the goniometer on the lateral surface of thigh and leg and the hinge of the goniometer at the level of knee. Other method is by keeping the arms of goniometer on the anterior surface of the thigh and leg and the hinge of goniometer over the centre of patella.
In patients with genu valgum one should do the Ober’s test to rule out ITB contracture and assess the patient for patellofemoral instability. Measure the standing height, sitting height and arm span of the patient.
Assessment of lower limb length discrepancy
- Limb length discrepancy(LLD) may be true or functional. True limb length discrepancy is due to shortening or lengthening of bone or joint dislocation. Functional LLD is due to abnormal joint positioning such as pelvic obliquity due to adduction contracture or flexion deformity of knee.
- LLD may be due to abnormal pelvic height, femoral length, tibial length or foot height. LLD may lead to abnormal gait, cosmetic problem, osteoarthritis due to abnormal weight transmission or low backache. LLD up to 2 cm at skeletal maturity is considered physiological as only about 25-30% of normal population have equal limb length. Left lower limb is longer than the right in a ratio of 3.5:1.
- When the patient is standing; assess whether the shoulder, iliac crest and the popliteal and the gluteal creases are at the same level. Look for compensatory scoliosis, which will disappear if the patient is made to sit. LLD may be masked by flexion of opposite knee and plantar flexion of ankle.
- LLD is best measured using blocks of known height under the foot of the affected side; till the pelvis is level and the compensatory lordosis disappears. Lower limb length measurement includes measurement of the whole lower limb and measurement of length of individual limb segments. Whole length measurement is done either by placing blocks of known thickness under the shorter limb till the pelvis is level or by measuring using a measuring tape.
- With measuring tape; measure both the true length and apparent length. Apparent length is measured from the xiphisternum or umbilicus to the inferior tip of the medial malleolus when the limbs are kept parallel. To measure the true length, both the limbs should be kept in an identical position. Hence if there is a fixed adduction deformity of hip; first make the pelvis level by adducting the affected hip till both the anterior superior iliac spines (ASIS) are at the same level. Measure the true length if the affected limb from the inferior edge of ASIS to the inferior edge of medial malleolus. Now keep the opposite hip also in an identical degree of adduction and then measure the other side as well.
- The lower limb has 4 segments; supratrochanteric (pelvic), infratrochanteric (femur), tibial and foot segments. Infratrochanteric segment is measured from the tip of greater trochanter to the lateral joint line of knee. Tibial segment is measured from the medial joint line of knee to the tip of medial malleolus.
- Supratrochanteric segment is measured by drawing the Bryant’s triangle, Nelaton’s line or Shoemaker’s line. Bryant’s triangle is drawn by drawing three lines in the supine position. First line from the inferior edge ASIS vertically down towards the examination table. Second line is drawn from the ASIS to the tip of greater trochanter. Third line is from tip of trochanter to the first line. Measure each sides of the triangle and compare with the other lower limb. Difference in the length of third line suggests supratrochanteric shortening. Supratrochanteric shortening may be due to hip arthritis, hip dislocation, fracture neck of femur or coxa vara.
Suggested reading
1. Pauwels F. Biomechanics of the locomotor apparatus. New York: Springer Verlag, 1980.
2. Chao EYS, Neluheni EVD, Hsu RWW, Paley D. Biomechanics of malalignment. Orth Clin N.A. 25: 379-386, 1994.
3. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J. Bone Joint Surg, 69A: 745-749, 1987.
4. Andriacchi TP. Dynamics of knee malalignment. Orth Clin N.A., 25: 395 406, 1984.
5. Paley D, Tetsworth K. Malalignment and realignment of the lower extremity. Orth Clin N. A., 25:355-367, 1994.
6. Paley D,Herzenberg JE,Tetsworth K et al. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425-465
7. Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am 1975;57:259-61
8. Bruce RW Jr. Torsional and angular deformities. Pediatric Clinics of North America 1996:43:867-81.
9. Staheli LT, Corbett M, Wyss G, King H. Lower extremity rotational problems in children. Normal values to guide management. J Bone Joint Surg Am 1985;67:39-47
Posted by Dr Rajesh Purushothaman, Associate Professor, Government Medical College, Kozhikode, Kerala, India
Good one and well descibed in brief.
Thanks to Dr Rajesh.
Very nice
Thank you rajesh sir. Very well given.