Courtesy: Orthopaedic Princples ICL Kochi by Dr Hitesh Gopalan
LISFRANC INJURIES
- Any bony or ligamentous injury involving the tarsometatarsal joint complex
- Named after the napolenic era surgeon who described amputations at this level without ever defining a specific injury
- Lisfranc joint articulation between the 3 cuneiforms and cuboid and the base of the 5 metatarsals
- Osseous stability is provided by the roman arch of the metatarsals and the recessed keystone of the second metatarsal base
- Lisfranc ligament :large oblique ligament that extends from the plantar aspect of the second metatarsal base and medial cuneiform
- Interoseeous ligament-connect the metatarsals through 5 metatarsal bases both dorsal and plantar(stronger and larger)
- Balancing ligaments: plantar fascia, peroneus longus and the intrinsics
- Associated structures:
1.dorsalis pedis artery:courses between first and second metatarsal bases
2.deep peroneal nerve:runs alongside the artery
INCIDENCE
- Generally considered rare (1 per 55,000)
- As index of suspicion increases, so does incidence
- Approximately 20 % Lisfranc’s injuries may be overlooked(especially in polytraumatised patients)
MECHANISMS OF INJURY
a. Trauma: motor vehicle accidents account for one third to two thirs of all cases(incidence of lower extremity foot trauma has increases the use of air bags)
b.Crush injuries
c.Sports related injuries are also occurring with increasing frequency
d.Direct injuries:force is applied directly to the lisfrancs articulation.the applied force is to the dorsum of the foot
e.Indirect injuries :more common than direct and result from axial loading /twisting,metatarsal bases dislocate dorsally more often than plantarly
f.twisting injuries: leading to forceful abduction of the forefoot, often resulting in a second metatarsal base fracture and /or compression fracture of the cuboid(nut cracker)
CLASSISFICATION
A. Homolateral
-all of the metatarsals are dislocated to the same side
-usually involves the second through 5th dislocated laterally
B.Divergent
-may be assosciated with a fracture of first cuneiform
Usually involves medial displacement of the first metatarsal and lateral displacement of 2nd -5th metatarsals
MODIFICATION
QUENU AND KUSS CLASSIFICATION
A. Homolateral-MOST COMMON
B. Isolated
C. Divergent
DIAGNOSIS
- Requires a high degree of clinical suspicion
1. 20% cases are the result of misdiagnosis
2. 40% cases have not received any treatment in the first week - Be wary of the diagnosis of midfoot sprain
CLINICAL FINDINGS
- Midfoot pain with difficulty in weight bearing
- Swelling across the dorsum of foot
- Deformity variable due to spontaneous reduction
- Ecchymosis may appear later
- Local tenderness at the tarsometatarsal joints
- Gentle stressing plantar/dorsiflexio and rotation will reveal instability
- Check neurovascular status for compromise of dorsalis pedis artery and/or deep peroneal nerve injury
- Assses for compartment syndrome
FRACTURE/DISLOCATION FINDINGS
- The most consistent finding is the misalignment along the medial side of second metatarsal and the second cuneiform
- The medial cuneiform-second metatarsal space should be evaluated for the fleck sign indicating the avulsion of the lisfranc ligament
RADIOGRAPHIC EVALUATION
- AP.lateral and 30 degree oblique xrays are mandatory
- AP:the medial margin of the second metatarsal base and medial margin of the middle cuneiform should be aligned
- OBLIQUE:medial base of the 4th metatarsal and medial margin of the cuboid should be aligned
- LATERAL:the dorsal surface of the first and second metatarsals should be level to the corresponding cuneiforms
- Standing views provide stress and may demonstrate subtle diastasis
- Comparison views are very helpful
ASSOSCIATED FRACTURES
1.base of second metatarsal
2.avulsion navicular
3.isolated medial cuneiform
4.cuboid
ADDITIONAL IMAGING
1.True stress views or fluoroscopy
2.CT scans
3.Bone scans-for the persistent pain with no radiographic findings
4.if suspicious: repeat x-rays and keep looking
TREATMENT
- Depends on severity
- RICE
- If no dislocation-Immobilise and no weight bearing for 4-8 weeks
- If significant dislocation-closed reduction or ORIF
OPERATIVE TREATMENT
Surgical emergencies
1.open fractures
2.vascular compromise
3.compartment syndrome
4.irreducible fractures
OPERATIVE TECHNIQUE
1-first incision centered at TMT joint and along axis of second ray lateral to EHL tendon
2-identify and protect neurovascular bundle
3.reduce and provisionally stabilize the second TMT joint
4.reduce and provisionally stabilize the first TMT joint
5.if lateral TMT joints remains displaced use 2nd and 3rd incisions
If reductions are anatomic, proceed with permanent fixation
1.screw fixation is preferable for medial column
2.pocket hole to prevent dorsal cortex fractures
3.screws are positional not lag
4.to aid reduction or if still unstable use a screw from medial cuneiform to base of second metatarsal
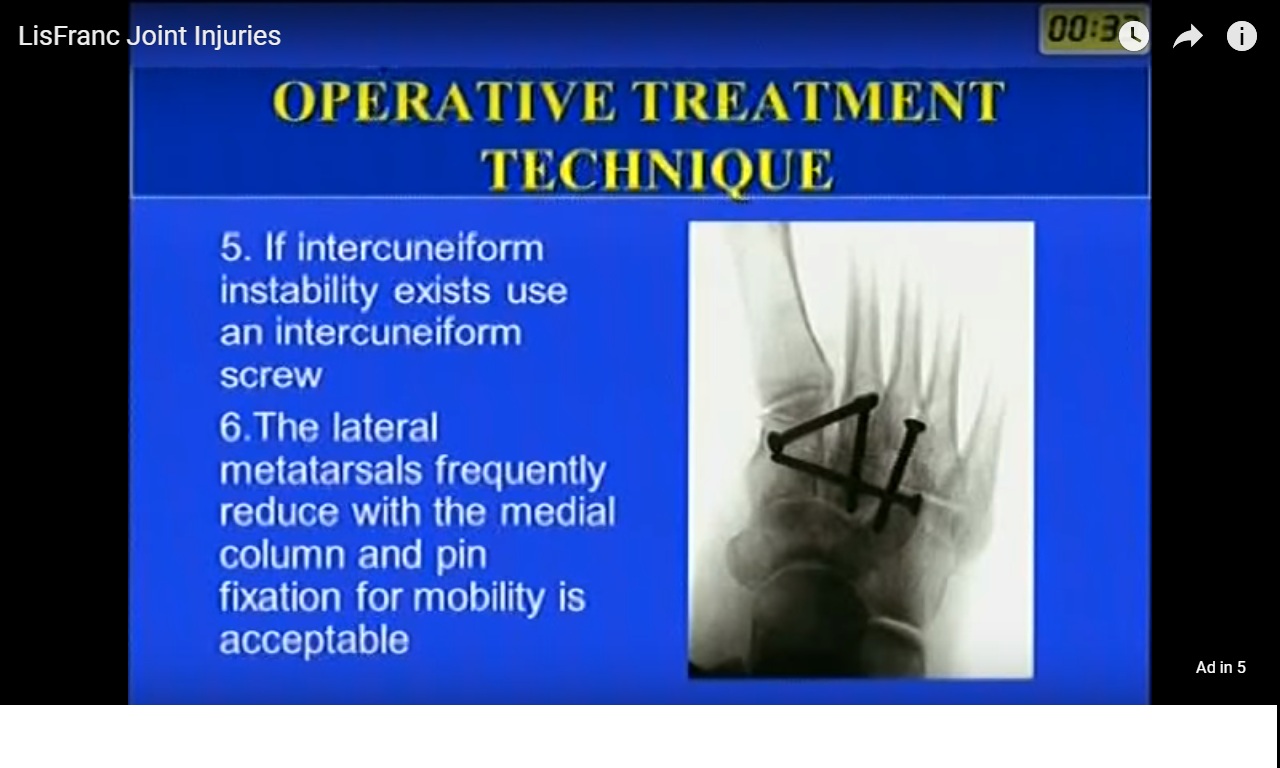
5.if intercuneiform instability exists use an intercuneiform screw
6.the lateral metatarsals frequently reduce with the medial column and pin fixation for mobility is acceptable
POST OPERATIVE MANAGEMENT
- Splint for 3 weeks
- Non weight bearing 4-6 weeks
- Arch support for 3-6 months
COMPLICATIONS
- Compartment syndrome
- Infection
- Chronic pain
- Neurovascular injury
- Hardware failure
PROGNOSIS
- Long rehabilitation(>1 year)
- Incomplete reduction leads to increased incidence of deformity and chronic foot pain
- Incidence of traumatic arthritis(0-58%) and related to intraarticular surface damage and comminution
Leave a Reply