A swelling in the popliteal fossa
Authors:
Tarun Goyal, Trust Registrar, Victoria Infirmary Hospital, Glasgow , UK
Sujit Kumar Tripathy, Clinical fellow, Southtees Hospital NHS Trust. UK
Q: A 22-year-old male presented with pain and gradually increasing swelling on the back of the knee for 6 months. He was a known case of haemophilia. There was no history of trauma preceding the swelling. There was no sudden increase in size of the swelling. There was no knee effusion. Range of knee motion was reduced to 0-90 degrees.
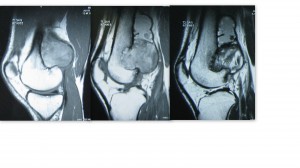
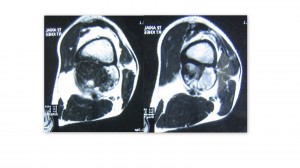
On examination there was a 10x 6cm mass in the popliteal fossa. It was firm in consistency, non mobile, deep to muscles and continuous with femur. Distal neurovascular status was intact. Radiographs showed a growth along the posterior femoral cortex with destruction of the cortical bone. This was confirmed on MRI scans.
Full blood count, renal and liver function tests were normal. Inflammatory markers (ESR, CRP), alkaline phosphatise and acid phosphatise were normal. Chest X-ray was normal. No abdominal pathology detected on USG. Factor VIII levels were more than 1%. Needle biopsy was obtained for histological diagnosis. The histology from the wall of the lesion revealed fibrous tissue with hemosiderin laden macrophages.
1. What is your diagnosis?
a. Haemophilic pseudotumor
b. Malignant fibrous histiocytoma
c. Parosteal osteosarcoma
d. Chondromyxoid fibroma
2. How you will treat the condition?
a. Factor VIII concentrate transfusion
b. Above Knee amputation
c. Radical excision + endoprosthesis
d. Complete marginal excision
3. What is the classification of Haemophilic arthropathy?
4. What is Synoviorthesis?
- The first correct answer will receive a copy of JP Stannard’s Orthopaedic Trauma from Thieme Publishers worth Rs 18,000/-Rs.
- Please send your answers only to mail@orthopaedicprinciples.com. Answers sent to this email alone will be taken into consideration.
- Please write your address along with the email.
- Winners of the Quiz will be announced on February 1, 2012
ANSWERS: Feb 1, 2012
Hemophiliac Pseudotumor
Sujit Kumar Tripathy, Clinical Fellow Orthopaedics, Friarage Hospital, UK
Tarun Goyal, Clinical Fellow Orthopaedics, Victoria Infirmary Hospital, Glasgow
1. What is haemophiliac pseudotumor?
- Hemophilic pseudotumors were first described in 1918 by Starker. Pseudotumors are an uncommon complication occurring in 1%–2% of persons with severe forms of haemophilia (clotting factor less than 1% of normal individual).
- Because, both hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency, or Christmas disease) are X-linked recessive genetic disorders, pseudotumors are found almost exclusively in men between 20 and 70 years of age.
- A hemophilic pseudotumor is an encapsulated, chronic, slowly expanding hematoma seen as a result of recurrent hemorrhage in extraarticular musculoskeletal systems. Many patients recall sustaining an injury prior to development of the pseudotumor.
- These lesions usually occur in soft tissues (often intramuscular) but occasionally occur de novo in bone (osseous) or in a subperiosteal location. Occasionally, however, they cross the anatomic boundaries.
- Pseudotumors that occur in muscles with broad tendon insertions readily progress to cause severe pressure erosion of adjacent bone. The bones most commonly involved by pseudotumors are the femur, pelvis, tibia, and bones of the hand.
2. What are the manifestations (clinical and radiological) of pseudotumor?
Clinical manifestation
- Progressive enlargement of a pseudotumor exerts more pressure on adjacent structures. Bones may be completely destroyed, and muscles and skin are often compressed and may undergo necrosis. Compartment syndromes and joint contractures may also occur.
- Pseudotumors are usually painless, but compression of nerves may produce pain or neurologic deficits. Pathologic fractures may also cause pain. Superimposed infection or fistula formation to skin or bowel frequently complicates disease management.
- With soft-tissue progression of a pseudotumor, there may be profound loss of function of the involved extremity. In rare instances, exsanguination has resulted from pseudotumor rupture. Patients with pseudotumors are often asymptomatic or stable for long periods of time, only to suddenly and unpredictably develop one or more of the complications described earlier.
Osseous pseudotumor
- Repetitive bleeding into the bones results in osseous pseudotumor, whereas repetitive bleeding into the joints leads to hemophilic arthropathy. Because of repetitive bleeding inside the bone, it leads to bone absorption and cystic degeneration.
- The bone marrow, joint capsule and the joint may get damaged or develop necrosis due to the mechanical and chemical stimulation by the cellulose, hemosiderin, and other substances in the blood. The rising intraosseous pressure may cause osteolytic bone destruction and the swelling damage. In some instances, the extreme swelling led to the breakthrough of the cortical bone.
- The pseudotumor often associated with soft tissue swelling and periosteal reaction. The hyperplasia of the periosteum may risk further damage. The pseudotumor occurred in the long bones can easily cause pathological bone fractures, which easily get misdiagnosed as the bone tumor if patient’s clinical history of easy bleeding was neglected.
- X-rays: The findings vary greatly with the extent, location, and different stages of hemorrhages and reflect the presence of medullary bone destruction, cortical changes, internal opacities, various types of periosteal reaction, and surrounding soft-tissue abnormalities. Osseous pseudotumors are lytic in nature and usually have a well-defined margin; however, they may become quite extensive and completely replace segments of bone. Lesions may be intramedullary or eccentric in location and are often expansile. Osseous trabeculae frequently traverse the lesions. Occasionally, calcific or ossific foci are present in the internal matrix; these foci are presumably dystrophic or sequestral in nature. There is often reactive sclerosis around bone pseudotumors.
- With these variable radiographic appearances, osseous hemophilic pseudotumors can be confused with other tumorous or infectious conditions. Hemophilic arthropathy near the pseudotumor is frequently found on conventional radiography.
Intraosseous pseudotumor
- X-rays: It looks like a well-defined, unilobular or multilobular, expansile lytic lesion of variable size, can occur in metadiaphysis or epiphysis, and have ventral or eccentric epicenters. They may show endosteal scalloping, cortical thinning or thickening, as well as peripheral sclerosis. Trabeculae or septalike structures frequently extend across the osteolytic lesions. Dystrophic calcification may be present. Progressive expansion may lead to deformity or pathologic fracture.
- Intraosseous pseudotumors simulate primary and secondary neoplasms (giant cell tumor, desmoplastic fibroma, plasmacytoma, metastasis), tumorlike lesions (solitary bone cyst, aneurysmal bone cyst, brown tumor), and even infection (echinococcosis).
- CT is particularly useful for the evaluation of crossing trabeculae, cortical change, and periosteal reaction.
- MRI has a remarkable ability for assessing intramedullary portions and nearby soft tissue (neurovascular bundle) as well as monitoring the therapeutic response. The characteristic MRI appearance is an intramedullary cystic lesion containing fluid components, which have complex signal intensities reflecting the effects of remote and recurrent hemorrhage and clot organization.
Subperiosteal pseudotumor
- It occurs secondary to hemorrhage that has caused elevation of the periosteum along the cortex and pressure necrosis of the bone. Immature skeleton is particularly easy to lift.
- X-rays: cortical erosion due to pressure, subperiosteal bone formation, and soft-tissue extension. Pseudotumors may also produce an aggressive periosteal reaction and curvilinear calcific strut that projects into soft tissue. Differential diagnosis includes Ewing’s sarcoma, metastasis, or infectious conditions.
- CT and MRI: hemorrhagic lesions may be confined to the subperiosteal space or extended to the intramedullary portion or soft tissue. The elevated periosteum is well visualized
Soft-Tissue Pseudotumor
- Repetitive bleeding into soft tissue which is not resolved and replaced by fibrous tissue causes joint contractures and soft tissue pseudotumors. Soft-tissue pseudotumors are most common in the thigh, gluteal region, and iliopsoas muscle.
- It can be categorised into intramuscular or extramuscular (interfascial, subcutaneous) pseudotumors. Osseous lesions may coexist in some cases.
- Intramuscular hematomas generally remain localized, although they may dissect along the muscle fibres to reach the bone and thereby produce remarkable pressure deformity or subperiosteal bone formation. Pressure to adjacent soft tissue may lead to skin necrosis, pain, neurologic deficits, and impaired mobility. Secondary infection is a rare phenomenon that can result from perforation into viscus or from an iatrogenic cause. In the case of iliopsoas pseudotumors, the retroperitoneal and intraperitoneal hemorrhage may be linked
- X-rays: It shows increased soft-tissue density, with or without internal calcification. Adjacent bony structures may be normal or show focal bone formation (may be seen only beneath the periosteum), extrinsic erosion, periosteal reaction, or medullary destruction. Gas in the pseudotumor suggests secondary infection.
- USG: Sonography is useful to follow the progression or regression of hematoma after therapy.
- CT Scan (with contrast): It can better delineate the outlines and wall thickness of the peripheral enhancing capsule. Variable patterns of both the echogenicity on sonography (anechoic or heterogeneously low) and attenuation on CT (high, isodense, or low) represent different stages of the hemorrhagic event.
- MRI: A heterogeneous signal in pseudotumors (as well as those in other locations) on both T1- and T2-weighted MR images reflects blood products in various stages of evolution. Acute hemorrhage (1–6 days) with intracellular deoxyhemoglobin appears isointense on T1-weighted images and hypointense on T2-weighted images. As the T1 relaxation time shortens (by methemoglobin) and RBCs break (> 7 days), the signal intensity progressively increases, from the periphery to the center, on both sequences [3]. A peripheral rim of dark signal intensity on all sequences is consistent with the fibrous capsule or hemosiderin. Intramuscular pseudotumor may show mural nodules at the capsular wall on MRI.
3. What are the histological characteristics of pseudotumor?
- A pseudotumor consists of blood products in various stages of evolution and has a fibrous capsule that contains hemosiderin-laden macrophages. Inflammatory cells such as polymorphs, lymphocytes, monocytes and macrophages may be found depending on the chronicity and infective condition of the pseudotumor.
4. What investigations will you plan?
- Laboratory investigations: full blood counts, coagulation profile, other basic haematological tests such as renal and liver function tests. Selective measurement of coagulation factors helps in assessing disease severity and also decides the treatment.
- Radiographs, USG, CT scan, MRI: these findings have already been described in respective sections.
- Angiography has been used on rare occasions for presurgical planning but can now probably be supplanted by CT or MR angiography. Angiographic findings confirm pseudotumors to be avascular.
| This 22-year-old man was suffering from a known condition of haemophilia. He developed a swelling in the popliteal fossa (posterior part of distal femur) that was gradually progressive without any manifestations of joint involvement. It was painless, there was no joint effusion and the restriction of knee movement was purely mechanical.
Spontaneous bleeding in haemophilia occurs when factor conc. becomes below 1%. However, moderate severe disease (1-5%) can bleed after trauma or repetitive minor-trauma. The factor conc. was more than 1% at the time of presentation in the index case. Needle biopsy is strictly avoided in pseudotumor to avoid potential complications. However under factor VIII control, one can perform needle aspiration (very small needle) to differentiate this condition from malignant lesions. The radiological picture and MRI of this patient is confirmatory of haemophiliac pseudotumor. As the swelling has not caused severe disability of the patient, he was treated with factor VIII infusion and observed. There is a group of haemophiliac patients who are not on factor treatment regularly. However they seek medical treatment once they develop a hematoma producing injury like a pseudotumor. Biopsy is not needed always and diagnosis is most of the time established by the clinical and radiological pictures. As described, if it becomes essential to distinguish from malignant lesions, needle biopsy (with small needle) can be undertaken after factor VIII infusion. The treatment of a pseudotumor depends on its growth behaviour and its effect. Physicians generally prefer to observe the pseudotumor and leave it alone if it’s not causing any problems. If action is required, embolization of the pseudotumor can be performed. However in cases of significant pain, damage to bones or other body parts, or persistent anemia because of bleeding into the pseudotumor—surgery becomes necessary. The pseudotumor is removed enbloc (which is extremely difficult). In some life and/or limb threatening conditions, limb salvage is not possible and amputation is performed. |
5. What are the differential diagnoses?
- The radiologic differential diagnosis for osseous pseudotumor is largely academic because a diagnosis of pseudotumor can be made confidently when characteristic imaging findings are seen in a patient with a severe coagulation disorder.
- There are many malignant bone tumors that may resemble a pseudotumor, including fibrosarcoma, plasmacytoma, malignant fibrous histiocytoma, telangiectatic osteosarcoma, ewing sarcoma and metastatic disease from primary tumors in the kidney, thyroid gland, or lung.
- Benign bone tumors such as aneurysmal bone cysts, solitary bone cysts, brown tumors, and desmoplastic fibroma are considerations, as well as unusual infectious processes such as echinococcosis. The hemorrhagic nature of osseous and soft-tissue pseudotumors is not helpful in making the diagnosis; many benign and malignant tumors of the bone and soft tissue with internal hemorrhage have been reported.
- Infection has to rule out.
6. How to treat this condition?
- Percutaneous drainage or biopsy of a pseudotumor is contraindicated due to the high prevalence of complications, including life-threatening bleeding, fistula formation, and infection. Therefore, it is vital that the radiologist make the diagnosis of pseudotumor based on patient history and imaging findings.
- Therapy for hemophilic pseudotumor is aimed at preserving function; however, no standard therapy exists.
- There are two-schools of thoughts for the treatment of pseudotumor.
- One group believes that conservative therapy with immobilization and clotting factor replacement (factor VIII infusion, cryoprecipitate) works best for pseudotumors resulting from recent hemorrhage, whereas surgical management yields the best results for pseudotumors that have been present for years or for those in which conservative measures have been ineffective.
- Other investigators recommend that surgery (amputation, joint replacement surgeries) be performed in most patients. Radiation therapy with doses of 10–20 Gy has been used only in patients who do not respond to conservative treatment and in whom surgery is contraindicated.
| Synoviorthesis, is a minimally invasive, therapeutic procedure for early chronic synovitis in persons with haemophilia. The procedure involves irradiation of a synovial membrane by intra-articular injection of radiocolloids (90yttrium and P32) to destroy inflamed synovial tissue. This is an alternative procedure to arthroscopic synoviectomy. |
Further reading:
1. Stan ford JM, James TT, Allen AM, Dixon LR. Hemophilic Pseudotumor: Radiologic-Pathologic Correlation. RadioGraphics 2003; 23: 853-56
- Brant E, Jordan H. Radiologic aspect of hemophilic pseudotumors in bone. AJR Am J Roentgenol 1972; 115:525-539.
- Hermann G, Gilbert M, Abdelwahab I. Hemophilia: evaluation of musculoskeletal involvement with CT, sonography, and MR imaging. AJR Am J Roentgenol 1992; 158:119-123.
- Aspelin P, Pettersson H, Sigurjonsson S, Nilsson I. Ultrasonographic examination of muscle hematomas in hemophiliacs. Acta Radiol 1984; 25:513-516.
- Gaary E, Gorlin J, Jaramillo D. Pseudotumor and arthropathy in the knees of a hemophiliac. Skeletal Radiol 1996; 25:85-87.
- Guidelines for the management of haemophilia. Published by the World Federation of Hemophilia ©World Federation of Hemophilia, 2005

What is the correct answer
Dear all,
this is the entire literature review on Haemophilic pseudotumour. So what would be the best answer for question no. 2?
Ok thanks Who is the winner….
The winner is Dr Dhananjaya Sabat, Asst Prof, Maulana Azad Medical College, NewDelhi
very interesting case
Intramuscular hemangioma to be considered, please reply sir