Reverse Shoulder Arthroplasty
Bijayendra Singh, Consultant Shoulder and Elbow Surgeon, UK.
Introduction:
- In patients who have lost use of their rotator cuff and develop arthritis, the standard shoulder replacement does not work as it requires normal functioning rotator cuff muscles.
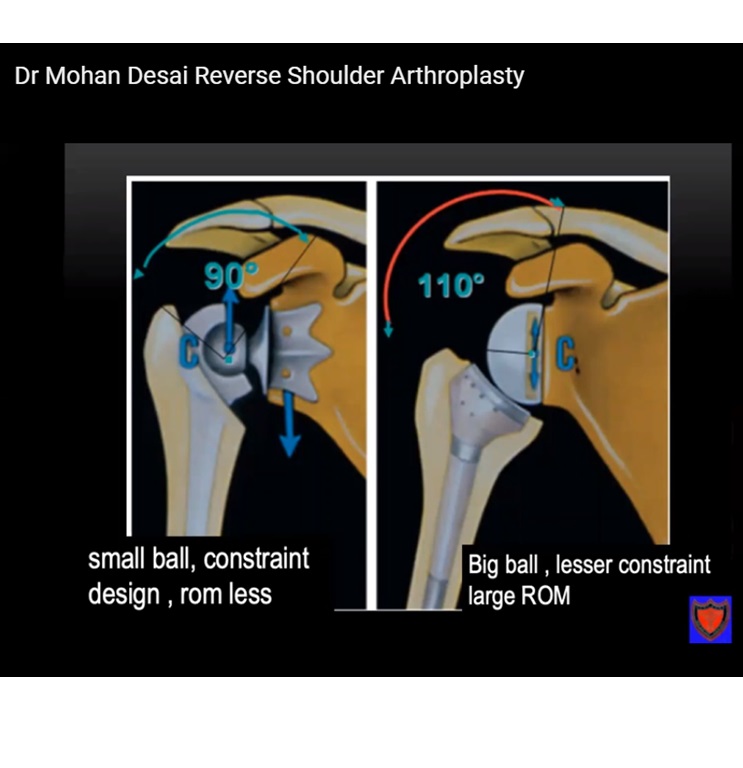
- This is a rather unusual solution to the problem of cuff tear arthropathy (arthritis). In this technique the ball & socket are switched around so that the socket is put on the ball side and the ball on the socket.
- This alters the way in which the deltoid works, enabling it to lift the shoulder without the help of the rotator cuff
- This type of implant was introduced by Charles Neer, who was also the first to search, albeit unsuccessfully, for solutions to the problem of damaged, fragile or absent peri-articular structures.
- Subsequently, semi-constrained or constrained implants were attempted in both anatomical and reverse forms but all the early prostheses resulted in implant failure with excessive constraint causing loosening of the glenoid component and poor functional results.
- In 1985 Paul Grammontdefined the bio-mechanical principles of medialization and lowering of the center of rotation of reverse shoulder prostheses and the importance of this new philosophy soon became clear.
Historical Perspective
- The first shoulder arthroplasty, performed in 1893 was a constrained prosthesis designed by the French surgeon Jules Emile Pean.
- The humeral stem was made of platinum and leather and it articulated with a head made of rubber coated with paraffin. The prosthesis was used to treat a case of tuberculosisbut while the functional results were reasonable, they were also short-lived and the prosthesis was removed two years later as a result of infection.
- There followed half a century without any reference to shoulder prostheses in the literature before Charles Neer performed the first simple, non-constrained humeral prosthesis in a case of fracture of the humeral head.
- This was a one block implant made of vitallium which reproduced the anatomy of the superior part of the humerus (Neer 1).
- Between 1950 and 1970, the indications for shoulder arthroplasty widened. As a result of the failure of non-constrained prostheses in cases where the rotator cuff was torn, Neer was drawn to consider new concepts that might be useful in such complicated cases. The lack of a rotator cuff can result in proximal migration of the prosthesis with eventual superior impingement, glenoid loosening and a poor functional outcome.
- In order to avoid this, various prostheses were designed in an attempt to increase the intrinsic stability of the implant with increasing conformity and constraint of its components.
- In the Neer Mark II prosthesisthe glenoid was modeled on the acetabulum. The English MacNab prosthesisand the DANA shoulder followed the same principles. However loosening of the glenoid component at short and medium term follow-up rendered these non-constrained prostheses unreliable and they were therefore abandoned.
- In a further variety, there was an attempt to mimic normal anatomy with a glenoid cup and a humeral head, a fixed center of rotation and a fixed fulcrum. In these prostheses the components were totally constrained.
- These early prostheses proved unsuitable in cases of shoulder arthropathy with irreparable rotator cuff tears. However, it was from these early failures that the principles of the reverse shoulder arthroplasty were born.
- The idea of the reverse shoulder prosthesis was introduced in the 1970s but initial trials were unsuccessful.
- Attempts to reproduce normal anatomy generated a number of complications. The pioneering work of Paul Grammont and the development of the DELTA III prosthesis have been fundamental to all subsequent shoulder arthroplasty systems.
- After more than 10 years of follow-up of these reverse prostheses, glenoid loosening remains a problem. This is a particularly difficult challenge given the frequent lack of glenoid bone stock. There is still room for innovation and progress in the treatment of arthritis associated with rotator cuff deficiency.
Biomechanics and Indications
- An intact rotator cuff produces a concavity compression, a mechanics that produces stability to an unconstrained joint.
- This provides a stable fulcrum so that the deltoid can rotate the humeral head and elevate the arm.
- A stable fulcrum requires intact coronal and transverse muscle force couples.
- the subscapularis and the infraspinatus produce a transverse force couple whereas the inferior portion of the rotator cuff on the humeral head produces the coronal force couple
- in small rotator cuff tears the deltoid overcomes the loss of force couple by increasing force
- In larger tears the force required by the deltoid increases, and instead of rotating the humeral head, the deltoid pulls the humerus superiorly, the sign referred to as humeral head escape sign( anterosuperior escape)
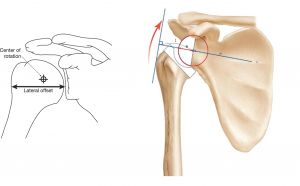
- RSA ( Reverse shoulder arthroplasty) acts by medialising the centre of rotation recruiting more deltoid fibres for forward elevation and abduction. Distalising the distal humerus increases the tension on the glenoid and a small lateral offset reduces the torque at the point of glenoid fixation
- The two common indications for RSA includes Massive rotator cuff tear with glenohumeral arthritis and Massive cuff tears with pseudoparalysis
- It is important to rule out two other conditions that may present as pseudoparalysis: cervical radiculopathy and deltoid dehisence, which will not be cured by RSA
- It is imperative to look for other signs of radiculopathy like biceps, triceps weakness, pain radiating to tip of fingers. Although external rotation deficit can be seen in C5 lesions, the external rotation deficit maynot be very severe as in cuff tears.
- Pseudoparalysis presents as sudden or progressive weakness with or without associated pain and a variable history of an antecedent trauma event.
- Care should be taken while selecting patients with good pre operative forward elevation more than 90 degree,especially in those with glenohumeral arthriti. Such patients will have high dissatisfaction rates following RSA. (Boileau P, J shoulder and elbow surgery 2009)
- Boileau is one of the few French surgeons who has designed the modern RSA and has extensive experience in the use of RSA. He dictates that RSA is best done in patients who are more than 70 years of age in the setting of advanced RCTA. It is also a good salvage option to save a failed Total Shoulder Arthroplasty or Shoulder Hemiarthroplasty.
Complications
- High complications have been reported in centres where RSA is performed infrequently(upto 20%). However in experienced hands the complications have been lower
- Complications include: scapular notching, instability, postoperative dislocation, infection, postoperative acromion fracture, glenosphere dissociation, periprosthetic fractures.
- Scapular notching leads to poor functional scores. Scapular notching can be minimised by placing the glenosphere more inferiorly and providing an inferior glenoid tilt.
Example
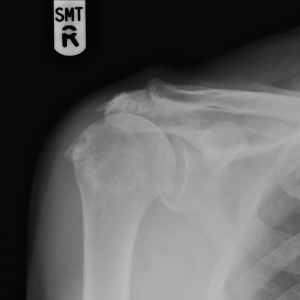
Preoperative radiograph of Chronic Rotator cuff tear Arthropathy
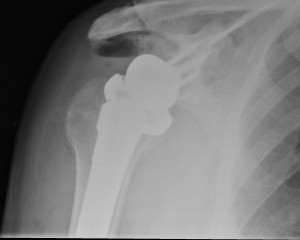
Potoperative radiographs after Reverse Total Shoulder Arthroplasty
AP view
lateral view
Courtesy:OrthoFRACS
Dr Ashish Babhulkar animated video on Reverse Shoulder Arthroplasty
Leave a Reply