FLEXOR TENDON INJURIES: PRINCIPLES OF MANAGEMENT
Flexor Tendon Zones(Verdan zones)
• Zone I extends from just distal to the insertion of the sublimis tendon to the site of insertion of the profundus tendon.
• Zone II is in the critical area of pulleys (Bunnell’s “no man’s land”) between the distal palmar crease and the insertion of the sublimis tendon.
• Zone III comprises the area of the lumbrical origin between the distal margin of the transverse carpal ligament and the beginning of the critical area of pulleys or first annulus.
• Zone IV is the zone covered by the transverse carpal ligament.
• Zone V is the zone proximal to the transverse carpal ligament and includes the forearm.
- The flexor tendons are covered by a thin visceral layer of adventitia, or paratenon.
- The tendons enter a synovium-lined fibro-osseous tunnel at the base of each digit that provides both a biomechanical advantage (on the basis of the pulley system) and a source of tendon nutrition (from the parietal and visceral layers of paratenon).
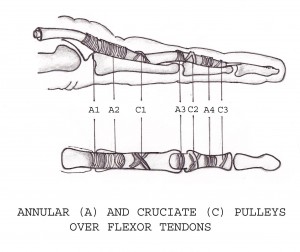
There is an arrangement of five annular pulleys and three cruciform pulleys in the finger.
1) The A1, A3, and A5 pulleys originate from the palmar plates of the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints, respectively.
2) The A2 and A4 pulleys are continuous with the periosteum of the proximal aspect of the proximal phalanx and of the middle third of the middle phalanx, respectively.
3) The cruciform pulleys are thin and compliant; they are located between the A2 and A3 pulleys (C1), between the A3 and A4 pulleys (C2), and between the A4 and A5 pulleys (C3).
EXAMINATION
Injured finger is stabilized for obtaining specific joint movements.
1) When proximal interphalangeal joint is stabilized, inability to flex distal interphalangeal joint suggest injury to the flexor digitorum profundus
2) Stabilizing metacarpophalangeal joint inability to flex both proximal and distal interphalangeal joint suggest injury to both flexor tendons.
3) To evaluate injury to flexor digitorum superficialis keep the adjacent fingers in complete extension. Inability to actively flex the injured finger suggests injury to flexor digitorum superficialis.
For checking the integrity of thumb flexors – flexor pollicis longus tendon, the metacarpophalangeal joint of the thumb is stabilized. If the flexor pollicis longus tendon is divided, flexion at the interphalangeal joint is absent.
SURGICAL REPAIR
Tendon healing occurs through extrinsic (activity of peripheral fibroblast) and intrinsic mechanism (activity of fibroblast derived from tendon). It occurs in three phases
1) Inflammatory (48 to 72 hours)
2) Fibroblastic (5 days to 4 week)
3) Remodelling (4 week to 3.5 months)
Strickland six characteristics of an ideal tendon repair:
(1) easy placement of sutures in the tendon,
(2) secure suture knots,
(3) smooth juncture of tendon ends,
(4) minimal gapping at the repair site,
(5) minimal interference with tendon vascularity, and
(6) sufficient strength throughout healing to permit application of early motion stress to
the tendon.
Urbaniak Classification of suture configuration for tendon repair
• Group 1 suture applies shearing force to tendon ends parallel to collagen bundles and results in weak repair.
Eg: Simple sutures
• Group 2: longitudinal pull of suture is converted to either oblique or transverse compressive force on tendon and strength of repair approaches strength of suture material.
Eg: Bunnel suture, Kessler suture
• Group 3: strongest union, loading of tendon applies compressive force of tendon to tendon at right angles to longitudinal shearing forces.
Eg: Pulvertaft repair (Fishmouth suture).
Principles of flexor tendon repair:
- Flexor tendons should be repaired at whatever level they are severed
- Whenever possible the repair should be done primarily. When delayed a tendon graft may be required
- A2 and A4 annular pulley areas of flexor sheaths should be preserved – prevents tendon bowstring and flexion deformity and excursion of tendion is preserved.
- Tendon laceration of 60% or more is treated as a complete transection.
- Laceration less than 60% is evaluated for the risk of triggering. If triggering is seen, the flap of tendon is smoothly débrided, and the flexor sheath is repaired to help avoid entrapment or triggering of the flap in the defect in the flexor sheath.
- Four to 6 strands is optimal. Strickland modification of the Kessler’s technique is the standard.
- Initially the dorsal epitenon sutures are placed, then the core sutures and then finally the volar epitenon sutures
- The diameter of suture is also directly proportional to the strength of the repair; 3.0 or 4.0 caliber nonabsorbable suture is recommended.
- Locking suture technique does not increase repair strength.
- Failure of the repair frequently occurs at the knot.
- Repair supplemented with a running circumferential epitendon suture technique increases the strength of the core stitch up to 50% and minimizes gapping.
- Suture technique must withstand gap formation of 3 mm at the repair site during the initial 3 weeks following repair.
Zone I:
- Contains only the FDP tendon
- The tendon may be directly repaired if the distal stump is large enough, or it may be reinserted to bone(preferably)
- Sutures(using Keith needles) through the tendon and through the bone are brought out over the dorsal aspect of the nail and tied(alternatively use a pull out button technique)
- Care must be taken not to advance the tendon more than 1 cm
- The finger cascade: Excessive trimming and advancement of the profundus tendon leading to flexed position of finger compared with other fingers.
- Quadriga effect: uneven tension applied to the common muscle belly of the flexor profundus tendons due to advancement of tendon leading to limited flexion of the remaining profundus tendons
Zone II:
- When both the superficialis and profundus tendons are divided, it is preferable to repair both tendons because greater digital independence of motion may be achieved
- Repair of FDS and FDP also diminishes the likelihood of proximal interphalangeal joint hyperextension deformity
- Core suture with two or more strands, locking component and buried knots is preffered.
- Care should be taken when the flexor sublimis has been injured in the area just proximal to the proximal interphalangeal joint and distally where the orientation of the proximal and distal portions of the tendon can be misinterpreted and repairs may be incorrectly done with the sublimis slips malrotated.
- Care also should be taken to deliver the flexor profundus tendon through the split portion of the flexor sublimis when the profundus tendon has retracted proximally.
- 18 to 25% of patients with flexor tendon repair requires tenolysis.
Zone III:
- Results are better because of the absence of the fibro osseous sheath
Zone IV:
- The area beneath the transverse carpal ligament, a z-lengthening release and repair of the transverse carpal ligament should be performed to prevent flexor tendon bowstringing
Zone V:
- Involving the musculotendinous junction are difficult to repair because muscle tissue will not hold suture. May necessitate multiple mattress sutures
Postoperatively:
– The wrist should be immobilized at approximately 10 degrees of flexion, the MCP joints at approximately 70 degrees of flexion, and the IP joints at neutral
– A program of passive ROM exercises should be initiated that decreases the adhesions at the repair site and enhances intrinsic tendon repair
– At 4–6 weeks following repair, active flexion and extension exercises are allowed as splinting is discontinued.
– At 6–8 weeks, passive extension exercises and isolated blocking is encouraged.
– After 8 weeks, the patient may begin flexion against resistance
– With four-strand techniques in an intelligent compliant patient active motion can be begun earlier for zone I and II injuries
Passive ROM protocols:
| Klienert traction | Duran Traction |
| Prevents patients from moving their digits against resistance | Uses a protective splint, but no elastic bands |
| Maintains the digits in a protective fashion | Passive flexion obtained by the therapist or with use of uninjured hand |
| Requires that the fingers are maintained in flexion using an elastic band that is attached to the level of the wrist | Decreases incidence of flexion contractures at the PIP joint. |
Ref:
- Kleinert HE, Verdan C. Report of the Committee on Tendon Injuries (International Federation of Societies for Surgery of the Hand). J Hand Surg [Am], 1983; 8: 794-8.
very good article with basics thnks
thanx for brief, simple & excellent article. only one thing can be discussed regarding repair of FDS in zone II inj. Sometimes repair of FDS here causes crowding at flexor sheath, greater adhesion formation & diminished excursion. So in case of injury within A2 pulley, is it better to resect FDS rather than repair?
Basics facts about Flexor Tendon Injuries
How Are Flexor Tendon Injuries Treated?
Flexor tendon injuries are repaired primarily whenever possible. Repair should be completed within 1 to 2 weeks after injury.
What Are the Causes of Flexor Tendon Injuries?
Flexor tendon injuries are most commonly caused by a sharp cut to the finger or palm. Rupture of the attachment of the tendon to the finger can also occur and is commonly associated with recreational sports (such as tackling in football when the tackler’s finger becomes entangled in the opponent’s jersey). Flexor tendon injuries can also occur as part of a more severe injury, such as due to power equipment.
What Are the Long-Term Outcomes of Flexor Tendon Injuries?
Outcome from flexor tendon injury and repair depends on several factors. These include type of injury (sharp or not, clean or contaminated), concurrent injuries or preexisting disabilities to the affected hand, and compliance of the patient with postoperative therapy.
Describe the Ideal Repair Technique
Repairs in the fingers and hand are performed with core sutures, most commonly of braided nylon or another polymer. One British study showed no difference between absorbable and nonabsorbable core suture. 1 Repairs can involve 2, 4, 6, or 8 strands to the core suture. Strength is increased with more strands, but outcomes are comparable, provided appropriate therapy is used postoperatively. A supplemental suture of the epitenon is often performed as well. This improves the glide of the tendon by decreasing the diameter of the repair site and may also increase the strength of the repair. Core suturing should also be relatively volar within the tendon to minimize disruption of intrinsic tendon vascularity.
What Are the Benefits of Postoperative Motion?
Postoperative motion therapy helps prevent adhesion of the repaired tendon to the surrounding structures, including the flex-or tendon sheath.
What Factors Affect Tendon Healing?
Quality of the tendon suture has a major impact on healing. Repairs that gap >3 mm during rehabilitation will go on to rupture. Quality of the wound bed and the proximal and distal ends of the lacerated tendon will also affect healing, with better intrinsic tendon blood supply promoting strength of repair versus extrinsic blood supply, which may lead to adhesions of the repaired tendon to the surrounding tissue. Extensive bench research has investigated the effect of multiple growth factors and peptides on tendon healing. None of these are as yet available for commercial use.
Describe the Rehabilitation
Rehabilitation consists of controlled motion in a supervised setting of hand therapy. Active motion protocols tend to be more popular, but equally good outcomes can be achieved with passive motion protocols. The goal of therapy is to produce tendon motion to prevent adhesion formation while minimizing stress on the repair, which may lead to gap formation and rupture.
What Complications Are Known to Occur After Treatment of Flexor Tendon Injuries?
In addition to the usual complications of surgery, flexor tendon repairs can be complicated by adhesion of the repaired tendon to the surrounding sheath and rupture. Injury to the A2 and/or A4 pulley, either during the initial injury or the surgical exploration, can lead to tendon bowstringing, which will decrease the recovery of motion for the finger.
What is the Effect of Seprafilm on Adhesion Formation and Tendon Healing?
Multiple agents, including Seprafilm (bilaminar hyaluronic acid and carboxymethylcellulose) (Genzyme Biosurgery, Cambridge, Massachusetts), have been investigated for their effects on adhesion formation prevention. This agent, and others including glycosaminoglycan gel, have been shown in some studies, primarily animal models, to decrease adhesion formation and work of flexion. There is not yet definitive evidence to advocate use of any agents or the superiority of 1 agent as compared to another.
What Does the Future Hold for the Treatment of Flexor Tendon Injuries?
Research is ongoing on the biology of tendon healing and how to positively effect it. Studies have evaluated application of various agents either placed between the repaired tendon ends or incorporated into the repair suture. In the future, as evidence to their effectiveness is generated, these may become available in commercial products.
excellent article for dnb final examinee,but littltle bit more stress on zone 2 repair should be emphasised.
Good article,it is short andsweet,very practical.
Thanks
Thanks,
great article,
I agree with one of the comments below.In case of Zon2 injury, It is hart to fit repaired both FDP and FDS tendons into the A2 pulley. I prefer to resect FDS in Zon2.
Excellent article with practical and relevant information for the Fellowship final as well as a quick reference for the on-call attendees.
It would have been a great help if u had put some more pics sir in most of the topics.. even in ur book .. information is really great but needs som more pics to catch easily