Tibial Plateau Fracture
Anatomical Pearls:
- The articular surface of the lateral tibial plateau is flat or slightly convex in relation to the medial tibial plateau that is concave, which provides greater congruity with the medial femoral condyle than on the lateral side.
- The lateral plateau is also higher than the medial plateau, accounting for the few degrees of varus of the tibial plateau in relation to the shaft.
- The most commonly used approaches for surgical fixation of tibial plateau fractures are the anterolateral approach and the posteromedial approach.
- Stronger, denser subchondral bone is found on the medial side due to increased load.
- The posterior cruciate ligament attaches about 1 cm below the joint line on the posterior ridge of the tibial plateau and a few millimeters lateral to the tibial tubercle.
Classification
Schatzker Classification
• Type I: Lateral plateau, split fracture
• Type II: Lateral plateau, split depression fracture
• Type III: Lateral plateau, depression fracture
• Type IV: Medial plateau fracture
• Type V: Bicondylar plateau fracture
• Type VI: Plateau fracture with metaphyseal –diaphyseal dissociation.
AO classification
A -non articular
A1.-avulsions
A2 – simple metaphyseal
A3 – comminuted metaphyseal
B – Partial articular
B1 – pure split
B2 – pure depression
B3 – split depression
C – complete articular
C1- simple
C2- articular simple, metaphyseal comminuted
C3- articular comminution
Biomechanics:
- The relative strength of the medial plateau, the valgus anatomic axis of the lower extremity, and the susceptibility of the leg to a medially directed force all lead to a prevalence of lateral-side injuries in low-energy fractures.
- Schatzker types I through III are low-energy injuries, whereas types IV through VI involve increasingly higher energy injuries
- Isolated medial plateau injuries represent more severe injury mechanisms
- Such injuries typically involve both lateral collateral and anterior cruciate ligament injuries and can result in a fracture dislocation of the knee
Clinical Features:
- Look for associated haemarthrosis
- An open wound may communicate with the knee joint. This can be identified by injecting 50cc of saline into the joint and looking for its appearance into the wound
- Watch out for compartment syndrome
- The ankle–brachial index of the extremity, along with ultra-sound examination of the leg, can be helpful in fully evaluating the possibility of vascular injury,
Imaging:
- Knee AP. Lateral, medial and lateral oblique views and 15° caudal view
- Coronal plane split fractures, which are commonly found within the medial plateau and are difficult to visualize on the anteroposterior projection alone and are best identified in a lateral view
- 3D CT helps to plan surgery
- MRI may help in identifying the status of the injured ligaments and menisci, but it doubtful whether this imaging will improve patient outcome.
- Traction radiographs provide ligamentotaxis to assist in a partial fracture reduction, preventing overlap of fragments and elucidating the fracture pattern.
Treatment
• Types I to III Schatzker:
– Non operative treatment for fractures, which are minimally displaced (<5 mm) and stable in varus-valgus stress test. Also for nonambulatory patients and surgically unfit patients. Mobilisation is begun on a hinged knee brace. Weight-bearing is delayed for 8- 12 weeks
– Depression or displacement exceeds 10 mm: surgery to elevate and restore the joint surface is indicated.
– When articular depression is between 5-10 mm, other factors like age, activity of the patient, associated injuries should be taken into account
– A fracture that is undisplaced initially and later gets displaced also needs surgery
– Also fracture with injury to collateral ligament which requires surgery needs ORIF.
– Similarly varus-valgus instability that exceeds 10° needs operative stabilisation
- Type IV to VI: Use of MIPPO (Minimally Invasive Percutaneous Plate Osteosynthesis) technique.
- In high energy injuries with significant soft tissue injuries, a temporary spanning external fixation maybe used initially and definitive fixation maybe delayed until the soft tissues heal (Anglen JO et al..)
- In high energy injuries, it is more important to restore overall joint congruity, coronal and sagittal plane alignment than obtaining perfect anatomical reduction of joint depression(Kettelkamp DB et al..)
- Limited ORIF uses Ligamentotaxis, to show which fragments can be restored without direct surgical intervention. Indirect reduction is achieved by Ligamentotaxis by external fixation or a femoral distractor or simple traction on the lower extremity.
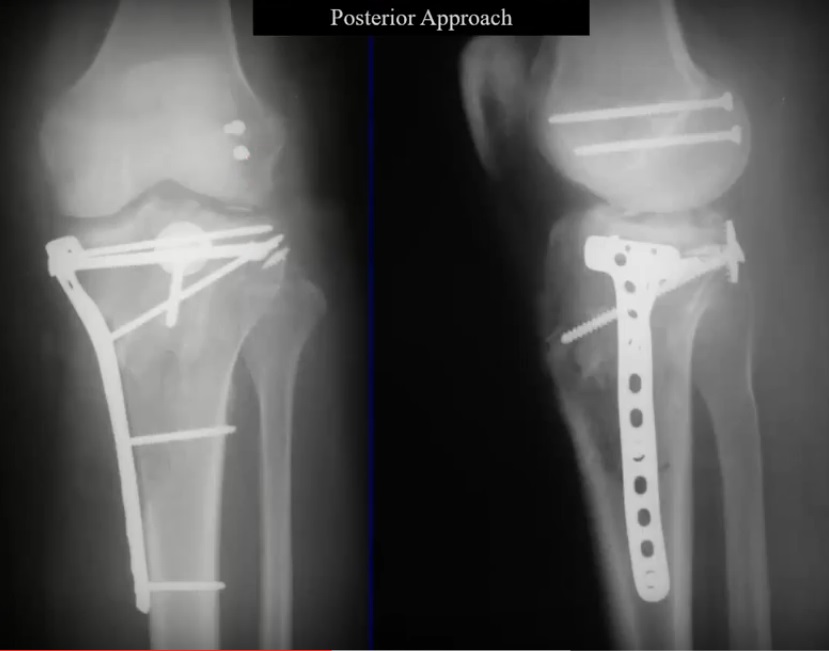
- The two most commonly used approached are the anterolateral approach and the posteromedial approach
– A submeniscal arthrotomy maybe done by incising the coronary ligament to evaluate the menisci and repair them
– The posteromedial approach is through the interval between the medial head of gastrocnemius and the pes anserinus tendons
– The posteromedial approach is used to reduce and fix the posteromedial fragment
– Extensile approaches through the anterior aspect of the knee(similar to TKA exposure) are less favoured for dual plating
- Partial incision of IT band will help to visualize further the lateral tibial plateau.
- Most of the meniscal injuries are peripheral rim tears and may be repaired in a horizontal mattress fashion to the capsule
- After reduction is achieved periarticular reduction clamps can be used to close the unicondylar or bicondylar fragments.
- Direct elevation of the depressed fragment may also be done
- The bone void that is created is restored with bone grafts or bone graft substitutes (calcium sulphate or calcium phosphate bone cements). Care must be taken not to allow extravasation of cement into the articular surface, hence screws must be placed before cement injection or when cement is in the moldable phase
- A periarticular plate (LCP) construct is used to fix the fragments
- An LCP may help avoid dual plating that is often done for Schatzker V and VI fracture subtypes.
– The medial condyle can be stabilized with lateral locking plates, provided multiple locking screws engage the medial fragment
– When compression is required between the medial and lateral fragment, nonlocked lag screws should be used before placing locked screws across the fracture line.
– But in the presence of a posteromedial fragment it will need fixation via an additional posteromedial approach.
– A minority of fractures, those with a bicondylar posterior shearing injury pattern, may benefit from a direct posterior exposure.
- Loss of articular reduction can be prevented by using multiple parallel screws in the subchondral area, these screws have been termed “raft screws”
- MIPPO: medial or lateral plating can be done depending on the type of injury. Plating is easier on the medial surface since the medial tibia is subcutaneous. On the lateral surface, the submuscular plane is identified and the plate is slid.
- Associated Ligament Injuries: Most authors agree that ligament(MCL/LCL) repair is not necessary in the acute setting
- Arthroscopically assisted reduction: advantages are treatment of associated ligament injuries and meniscal injuries.
– A potential complication of this technique is extravasation of arthroscopy fluid into the lower extremity compartment and risk for compartment syndrome.
– The risk of fluid extravasation can be minimized by going dry during the reduction stage and by making an incision where the plate or screws will be placed to allow the fluid to escape
Ref:
- Anglen JO, Aleto T: Temporary transarticular external fixation of the knee and ankle. J Orthop Trauma 1998; 12: 431-434.
- Kettelkamp DB, Hillberry BM, Murrish DE, Heck DA: Degenerative arthritis of the knee secondary to fracture malunion. Clin Orthop 1988; 234:159-169.
- Mueller KL, Karunakar MA, Frankenburg EP, Scott DS: Bicondylar tibial plateau fractures: A biomechanical study. Clin Orthop 2003;412:189- 195.
- Goesling T, Frenk A, Appenzeller A, Garapati R, Marti A, Krettek C: LISS PLT: Design, mechanical and biomechanical characteristics. Injury 2003; 34(suppl 1):A11-A15.
Very good reading here