FEMOROACETABULAR IMPINGEMENT
S Saseendar, Hitesh Gopalan U
Introduction
‘Femoroacetabular impingement(FAI)’ is a relatively recently described term which implies a subtle abnormality in either or both of the proximal femur and acetabulum causes interference in the normal movement between the two.
However the concept of FAI is not entirely novel as Stulberg et al addressed this entity as the ‘pistol grip deformity’ in describing the abnormal morphology of the femoral head and neck on anteroposterior (AP) radiographs of patients with early OA. However, impingement was recently popularized as the possible cause of OA in the young.
Based on the pathology, it can be classified as
A) Congenital – most common (acetabular retroversion,) or
B) Acquired (femoral neck fracture, following femoral osteotomy or periacetabular osteotomy, slipped capital femoral epiphysis, Legg-Calvé-Perthes disease)
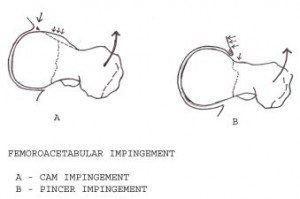
The more commonly used classification is that of Ganz et al who classified Femoroacetabular impingement into two distinct types based on the morphology of the femoral head and acetabulum:
A) The Cam type and
B) The Pincer type
Cam Impingement
Cam literally means the projecting part of a cog-wheel. Cam deformity, also called the ‘pistol grip deformity’ or the ‘head tilt deformity’ refers to an abnormal bony bump at the head neck junction of the femur. This nonspherical portion is usually found anterosuperiorly. This abnormal ‘bump’ or insufficient concavity of the femoral head-neck junction decreases femoral head-neck offset and causes impingement on the acetabular labrum and articular cartilage with daily activities.
The pure cam lesion most often occurs in active young men in their 20s to 40s. Continued impingement when the raised lesion of the femoral neck contacts the acetabulum causes delamination of the articular cartilage of the anterosuperior aspect of the acetabulum. The labrum is displaced outwardly and superiorly, eventually causing a clean, articular-sided labral tear. The delamination associated with the cam impingement and the larger area of cartilage damage result in a worse prognosis compared to the isolated pincer impingement.
Pincer Impingement
- Pincer impingement is an acetabular sided morphologic abnormality characterized by overcoverage of the femoral head.
- Isolated pincer impingement usually occurs in middle-aged women.
- Unlike cam impingement, the labral lesion tends to occur before the articular cartilage damage.
- The femoral neck makes contact with the acetabulum during normal motion due to the overcoverage.
- This crushes the labrum causing multiple intrasubstance cleavage tears and occasionally associated paralabral cysts unlike in the cam lesion where the labrum has a clean tear at the articular side.
- With time, a focal area of articular cartilage behind it becomes damaged.
- However, there is no delamination of the cartilage unlike in the cam impingement.
- Healing of the labrum creates an ossified rim, further worsening the acetabular overcoverage.
- With advanced disease, the head of femur levers on the overhanging anterosuperior acetabular rim (fulcrum) creating a posteroinferior counter-coup lesion. This is a late finding and carries a poor prognosis.
The overcoverage in the pincer deformity may be
A) ‘focal’ eg. acetabular retroversion (most common cause of pincer impingement), overcorrection during periacetabular osteotomy or
B) ‘global’ eg. coxa profunda or protrusion acetabuli.
Though Ganz et al classified femoroacetabular impingement into these two classic types, it has been shown by Beck et al that these two forms coexist in a large percentage of cases.
Clinical features
- The patient is usually an active young adult with slow onset groin pain that may start after a minor trauma.
- Pain is exacerbated with athletic activities or prolonged walking or sitting for a prolonged period.
- This is because impingement tends to occur with hip flexion and internal rotation.
- Pain may also be referred to the knee causing diagnostic difficulty.
Examination
Gait is slightly antalgic gait. Typically, the patient has <20o of internal rotation with the hip in 90o of flexion.
Anterior impingement test:
- It is almost always positive.
- This test is done with the patient supine; the hip is internally rotated as it is passively flexed to approximately 90° and adducted.
- This causes approximation of the femoral neck and the acetabular rim and recreates the pain.
Posteroinferior impingement test:
- It is positive in the presence of a posteroinferior impingement as in global overcoverage.
- The patient lies supine on the edge of the bed and the legs are made to hang free from the end of the bed in order to produce maximum hip extension.
- External rotation with the hip in extension produces severe, deep-seated groin pain due to posteroinferior impingement.
Imaging
Radiological examination
The lesions found in FAI are subtle and warrant special radiographs.
A) Radiologic evaluation of Pincer impingement
In order to accurately evaluate for pincer impingement a true anteroposterior
(AP) pelvis view should be obtained: the center of the sacrum and coccyx should be in line with the center of the pubic symphysis and the sacrococcygeal junction should be within 32 mm of the top of the pubic symphysis in men and 47 mm in women.
- Radiologic signs of ‘focal’ overcoverage (acetabular retroversion)
a) The crossover or figure-of-eight sign: Normally, the posterior rim of acetabulum should be lateral to the anterior wall on an AP view of the pelvis. In retroverted acetabulum, the anterior wall appears to “cross over” the posterior wall. The degree of retroversion can be inferred from where the crossover occurs.
Mild retroversion: Crossover occurs in the top third of the acetabulum
Moderate retroversion: Crossover occurs in the middle third
Severe retroversion: Crossover occurs in the inferior third
(Note: When one starts in the most inferior part of the acetabulum, the most lateral wall is the posterior wall.)
b) The ischial spine sign: It is a secondary sign of acetabular retroversion. In a true AP image of the pelvis, the ischial spines should not project into the pelvis; if so, one should look for other signs of retroversion.
c) The posterior wall sign: Normally the center of the femoral head lies medial to the posterior wall. When it lies lateral to the posterior wall, the posterior wall sign is said to be positive and implies a retroverted acetabulum. The sign also reflects how much posterior wall coverage exists.
- Radiologic signs of ‘global’ overcoverage (profunda, protrusio)
In a normal hip, the floor of the acetabulum, as represented by the acetabular teardrop, should be lateral to the illioischial line.
In coxa profunda, the teardrop touches or crosses over the ilioischial line but the femoral head does not.
In protrusio acetabuli, a more severe form of global overcoverage, both the teardrop and the femoral head cross the illioischial line.
B) Radiologic evaluation of Cam impingement
Identifying cam impingement requires special radiographs to view the femoral head neck junction. These include the cross leg lateral view in 15o internal rotation, the standard Dunn view (AP radiograph of the hip in neutral rotation, 20o of abduction, and 90o of flexion), and the modified Dunn view(AP radiograph of the hip in neutral rotation, 20o of abduction, and 45o of flexion). The modified Dunn view is the most sensitive.
a) The junction of the femoral head and neck should have a smooth contour from a concave to a convex morphology. Subtle lesions can be better appreciated by drawing a circle to fill the femoral head to highlight the head-neck junction. Any bony protrusion beyond this circle is suggestive of a cam lesion.
b) Alpha angle: Most cam lesions occur on the anterosuperior aspect of the femoral neck and are easily missed. The alpha angle is a sensitive method of diagnosing cam lesions. A line is drawn down the center of the femoral neck to the center of the femoral head. Another line is drawn from the center of the femoral head to the head-neck junction (Figure 10). The resulting angle is the alpha angle. The normal average is 42o while >50.5o is taken as diagnostic of cam impingement.
c) The head-neck offset ratio: The offset ratio is measured by dividing the anterior offset by the femoral head diameter. The anterior offset is the distance between two parallel lines, one adjacent to the anterior aspect of the neck and the other touching the most anterior part of the femoral head and both parallel to the femoral neck axis. A head-neck offset ratio of <0.15 on a cross-table lateral radiograph is 68% sensitive and 82% specific for the diagnosis of cam impingement.
Computed Tomography: Computed tomography scans provide a three-dimensional picture of the deformity and aid in determining the area of resection to correct femoral head asphericity.
Magnetic Resonance Imaging with gadolinium arthrography can demonstrate abnormalities of the acetabular rim such as labral tears, paralabral cysts, cartilage delamination, ossification of the acetabular rim and those of the proximal femur including abnormal sphericity of the femoral head and fibrocystic changes at the femoral head-neck junction (also known as Pitt’s pit). However MRI arthrograms cannot detect undetached chondral separations.
Management
Nonsurgical Treatment
- Initial trial of nonsurgical treatment includes activity modification including restriction of athletic activities, and nonsteroidal anti-inflammatory medications.
- Passive range of motion or stretching is largely counterproductive and exacerbates the symptoms.
- Nonsurgical treatment is only temporarily successful because of the young age and typically high activity level of the patients.
- Hence early surgical treatment is usually preferred.
Indications and contraindications
The mode of surgical treatment depends on
(1) the physiological age of the patient; (2) joint space narrowing of 1 to 2 mm; (3) the extent of damage to the acetabular labral chondral complex; (4) the severity of acetabular retroversion in pincer impingement and (5) the extent of head asphericity and the absence or presence of proximal femoral deformity (eg. high-riding greater trochanter) in cam impingement. A joint space reduction of 2 mm or more is best treated by joint replacement.
Surgical techniques for the treatment of femoroacetabular impingement can be broadly classified into three categories:
(1) Surgical dislocation of the hip and for complete exposure and correction of cam impingement and/or trimming of the acetabular rim,
(2) Correction by arthroscopy with or without arthrotomy (but without dislocation of the femoral head) and
(3) Periacetabular osteotomy for focal overcoverage
Surgical Dislocation of the Hip
Indications:
(1) Cam-type impingement with or without proximal femoral deformity,
(2) Pincer-type impingement associated with cam-type deformity and
(3) Cam impingement with 1 mm of joint space narrowing as this approach would allow conversion to arthroplasty if needed.
The technique for surgical dislocation was developed by Ganz et al and enables protection of femoral head vascularity wile providing complete exposure.
Periacetabular Osteotomy
Indication:
Acetabular retroversion with an associated posterior wall sign.
The cartilage in the anterosuperior aspect of the acetabulum must be intact for a periacetabular osteotomy to be recommended; if it is not intact, acetabular reorientation will place poor cartilage in the main weightbearing area.
Pincer impingement due to relative prominence of the anterior wall (the crossover sign) with an absent posterior wall sign (i.e., with the lateral aspect of the posterior wall lateral to the center of the femoral head) is best addressed with localized trimming of the rim, whereas coxa profunda requires global rim trimming. Both procedures are best done after surgical dislocation.
Hip Arthroscopy
Indications:
(1) cam-type impingement without proximal femoral deformity and
(2) isolated acetabular retroversion with or without cam-type deformity.
Advantages of arthroscopy: Smaller incisions, shorter recovery time and a lower morbidity rate.
Arthroscopy of the hip consists of two components namely arthroscopy of the central compartment (labrum and all parts medial to it) and arthroscopy of the peripheral compartment (everything lateral to the labrum within the capsule and includes the head-neck junction).
Arthroscopy of the central compartment is performed with traction. Labrum can be debrided and repaired. Delaminated cartilage can be excised, and exposed acetabular subchondral bone can undergo microfracture.
Arthroscopy of the peripheral compartment which is done through an anterolateral portal without traction enables reshaping of the femoral head-neck junction and removal of peripheral osteophytes.
Limitations of arthroscopy:
- Incomplete visualization leading to undertreatment or excessive removal of bone at the femoral head-neck junction and subsequent fracture.
- Neurovascular injury can be related to the entry portals eg. superior gluteal nerve with an anterolateral portal and the lateral femoral cutaneous and femoral nerves with an anterior portal or to the traction (affects sciatic and pudendal nerves).
- Steep learning curve
- Hip Arthroscopy can be combined with a mini-anterior (Hueter) hip arthrotomy to facilitate treatment of labral and chondral pathology and correction of cam deformity. The risk of an inadequate osseous correction is minimized.
References:
- Lucas Rylander, John M. Froelich, Wendy Novicoff, Khaled Saleh,: Femoroacetabular Impingement and Acetabular Labral Tears. Orthopedics: doi: 10.3928/01477447-20100329-21.
- Javad Parvizi, Michael Leunig, Reinhold Ganz: Femoroacetabular Impingement. J Am Acad Orthop Surg 2007;15:561-570.
- Paul E. Beaulé, David J. Allen, John C. Clohisy, Perry Schoenecker, Michael Leunig: The Young Adult with Hip Impingement: Deciding on the Optimal Intervention. J Bone Joint Surg Am. 2009;91:210-221.
- John C. Clohisy, John C. Carlisle, Paul E. Beaulé, Young-Jo Kim, Robert T. Trousdale, Rafael J. Sierra, Michael Leunig, Perry L. Schoenecker, Michael B. Millis: A Systematic Approach to thePlain Radiographic Evaluation of the Young Adult Hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47-66.
- Dalia A. Fadul, John A. Carrino: Imaging of Femoroacetabular Impingement. J Bone Joint Surg Am. 2009;91 Suppl 1:138-43.
- John C. Clohisy, Paul E. Beaulé, Aran O’Malley, Marc R. Safran, Perry Schoenecker: AOA Symposium. Hip Disease in the Young Adult: Current Concepts of Etiology and Surgical Treatment. J Bone Joint Surg Am. 2008;90:2267-2281.
- R. Ganz, T. J. Gill, E. Gautier, K. Ganz, N. Krügel, U. Berlemann: Surgical dislocation of the adult hip. J Bone Joint Surg [Br] 2001;83-B:1119-1124.
well written, Saseendar and Hitesh…u have nicely summarized the whole topic.. i ll just add on few things…nothing new…
Well the often quoted statement is actually quite helpful. “FAI is not a cause of hip pain!” FAI is a morphologic condition that the predisposes hip to intraarticular pathology that then becomes painful. So whenever we tell about FAI there are two parts to it.. the morphology and the intra-articular pathology.
Under the morphology heading we have our 1) Classification (pincer , cam), 2) x ray findings and 3)the “present” gold standard of morphology, 3D CT. what all of these do tell us is that patient has an altered anatomy, but what they don’t tell is that whether that’s causing the pain!
Under the intraarticular pathology (that causes pain) we have 1) clinical signs 2) MRI and 3) the present gold standard; – arthroscopy/ open
Essentially it will be helpful if we don’t mix these headings..for eg; never try using scopy / MRI for diagnosing the type of FAI (use xray or even better 3D CT before u scope or do MRI). or in other words understand the altered morphology before u look for the pathology that it caused ( get ur 3D CT before u scope!)
Now its helpful to remember what should normally happen when hip flexes . two things 1) the labrum that over hangs the acetabular bone like a flap should yield easily 2) the head/ neck junction has no business inside the acetabulum . In pincer the first doesn’t happen as the acetabular bone over grown over the labrum crushes it against femoral neck . Result is labral damage. In cam the second rule is breached and bony prominence of anterolateral femoral head/neck junction shears off the articular cartilage inside. Result is selective articular delamination ( Peel back) & relative labral preservation . so that makes it clear why pincers have labral problem and cams have articular problem
Few notes on scopy
Pincer
1) Anterior portal can be difficult cuz of the over hanging bone
2) Morphology (pincer)is managed by excision of bone . how much to take? Normal acetabulum starts at articulo labral junction. So that’s the margin
3) Pathology (labral); debride or repair? repair is better than debridement if the tissue is healthy and if repair doesn’t violate articular cartilage . like bankart’s mobilize the labrum from the capsular side and anchor is placed at articular end of labrum
Cam
1) what to do first? Pathology is addressed first (central comprtment under traction)
2) Morphology is managed next (Femoroplasty). For it ,a) anterior capsulotomy between anterior and lateral portal b) release traction & c) flex hip to 35 deg (more will cause FAI !)……then a) overlying fibrocatillage(it covers the cam lesion) is debrided b) remove bone as indicated in 3D CT and c) beware of notching!!! (learning curve !)
i found this to be an interesting article…almost like a screening test for FAI in young N. V. Bardakos et al; 43 hips with cam impingement followed up for 10 yrs, 28/43 showed OA progression, JBJS [Br] 2009;91-B:162-9.
Thanks. That was a wonderful and lively explanation of FAI by you Sir.
Really a very good & comprehensive data about FAI. Recently we had 2 patients at our clinic with c/o hip pain & we were suspecting FAI & thought about going again through FAI details & i found this article which is very helpful.
Thanks…….