IDIOPATHIC SCOLIOSIS
Rishi Mugesh Kanna, MS, MRCS, FNB(spine), Spine Surgeon, Ganga Hospital, Coimbatore, India
Introduction
Scoliosis refers to lateral curvature of the spinal column of more than 10 degrees when observed through an antero-posterior radiograph of the spine. There are different causes of scoliosis and the causes vary depending on the age of onset. In the pediatric age group, scoliosis can occur due to congenital anomalies of the vertebral body (congenital scoliosis), associated with intraspinal cord anomalies such as syrinx (secondary scoliosis) or can present without any identifiable etiology (idiopathic scoliosis).
Idiopathic scoliosis is the most common type of all forms of scoliosis. It is defined as a coronal plane spinal deformity characterized by lateral bending and fixed rotation of the spine in the absence of any known cause with a Cobb angle of 10° or more. Idiopathic, as the word refers to, the exact etiology of the disease is not known. Possible causes would include genetic factors, hormonal imbalance, biomechanical factors and connective tissue abnormalities. Although genetic basis for the causation of scoliosis has not been detected, the preponderance of a curve to develop curve progression has been recently identified by genetic tests (Scoliscore tests®).
Traditionally idiopathic scoliosis is classified according to age at onset into infantile (birth–3 years), juvenile (3–10 years), and adolescent (after 10 years) subtypes. This is based on the different patterns of curve characteristics like age at onset, side predilection, gender differences, regional differences in the spine etc. This classification is descriptive but does not help in planning the management of these patients. Recent alternative classification distinguishes pediatric scoliosis as early-onset scoliosis (0–5 years) and late-onset scoliosis (after 5 years) based on the differences in management protocols. Children with early onset scoliosis have a higher chance of progression, increased cardiopulmonary risk, weak spinal anchors for fixation and are best treated by non-fusion surgeries. Patients with late onset scoliosis are best treated by definitive corrective surgery with fusion.
Infantile idiopathic scoliosis
When scoliosis is detected before three years of age in the absence of congenital vertebral anomalies, it is called as infantile scoliosis. Male children are commonly affected. Left thoracic curve pattern is the most common. This condition has been associated with plagiocephaly, developmental delay, congenital heart disease, and developmental hip dysplasia. The association with plagiocephaly and hip dysplasia points towards a possible intra uterine positional abnormality as the etiology of infantile scoliosis.
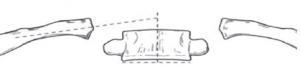
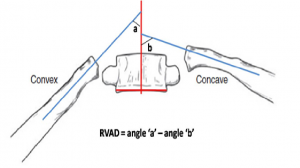
Two sub-types have been identified: a resolving type (85%) and a progressive type (15%). Resolving and progressive curve types are distinguished by analyzing the relationship between the apical vertebra of the thoracic curve and its ribs on an antero-posterior (AP) radiograph. Two radiographic parameters are used to analyse this relationship: the rib-vertebral angle difference (RVAD) and the rib phase. To assess RVAD, the rib vertebral angle is calculated first (Fig 1). This is determined by a line perpendicular to the endplate of the apical vertebra and a line drawn along the center of the rib. The RVAD is derived by subtracting the angle of the convex side from the concave side (Fig 2). An RVAD greater than 20° indicates that curve progression is likely.
Figure 1: Rib vertebral angle
Figure 2: Calculating Rib vertebral angle difference
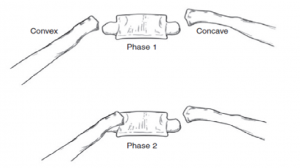
The rib phase is the second radiographic parameter and it is assessed by determining the amount of overlap between the convex rib head and the apical vertebral body. If the convex rib does not overlap the vertebral body (phase 1), progression is unlikely. As the curve increases, the apical convex rib overlaps the vertebral body (phase 2) and further curve progression is likely. Phase 2 ribs indicate that the rotation of the apical vertebra is severe and hence more likely to progress (Fig 3).
Figure 3: Rib Phase- Note the overlap of the convex rib head on the antero-posterior radiograph
Resolving curves are observed with serial physical examinations and radiographic monitoring. Sleeping in the prone position is recommended because supine positioning has been associated with infantile curves. Progressive curves are treated with serial casting under general anaesthesia followed by orthotic treatment with a Milwaukee brace. Curves that continue to progress despite orthotic treatment and those with more than 45 degrees at presentation require surgery. Since lung alveolar growth reaches full maturity at 8 years of age, it is essential to maintain spinal growth at least till 8 years. Hence non-fusion surgeries including posterior spinal instrumentation without fusion or the vertically expandable prosthetic titanium rib (VEPTR) are preferred in these patients. Both are growth-preserving procedures that permit delay of definitive fusion until the child has achieved additional growth. Posterior fusion surgeries also entail the risk of crankshaft phenomenon. Crankshaft phenomenon refers to persistent anterior spinal growth in the presence of a posterior fusion which can lead to recurrent and worsening spinal deformity.
Juvenile idiopathic scoliosis
Juvenile idiopathic scoliosis actually represents a sub-group of adolescent idiopathic scoliosis patients, who have presented at an earlier age. So their clinical and radiological features are similar to adolescent scoliosis. As in AIS, female children are predominantly affected and right thoracic and double major curve types are common. Since they present before the peak growth spurt, they have a high tendency to progress (up to 70% of curves progress).
Orthotic treatment is advised for curves in the 25° to 50° range. Surgical treatment is considered when curve magnitude exceeds 50° to 60°. Surgical decision making is complex and concerns include the remaining growth and potential for development of crankshaft phenomenon. Non-fusion techniques such as growing rod instrumentation are considered for patients less than 10 years of age with severe curves. Single-stage posterior spinal instrumentation and fusion using segmental pedicle fixation and combined anterior and posterior fusion with posterior instrumentation is an option for older patients.
Adolescent idiopathic scoliosis
This is the most common type of scoliosis in children and the general prevalence is 3%. But only less than 0.3% of patients develop curves requiring surgical treatment and most other curves do not progress.
Clinical evaluation:
A female predominance is noted, which increases substantially for larger curves. Thoracic curves are more common than the lumbar curves. Thoracic curve patterns are generally convex to the right and lumbar curves are convex to the left. This pattern is so common in AIS that variations of this type are an indication for MRI examination to look for spinal cord anomalies. Children are usually brought by the parents for cosmetic concerns, and pain is an uncommon presenting symptom. Neurological symptoms are rare even in very severe curves. Patient history should include menstrual history, birth and developmental history and family history of scoliosis.
In the physical examination, the patients are examined for facial syndromic features such as frontal bossing, hypertelorism, high arched palate etc. The spine is examined from behind and any asymmetry of the shoulder, thorax and waist is looked for. Adams forward bend test is a useful screening test to diagnose scoliosis. The patient is asked to bend forward to look for any rib or loin hump (Fig 4). Normally the right and left sides of the trunk should be symmetrical. Presence of a thoracic or lumbar prominence suggests scoliosis. The back is also examined for neurocutaneous markers such as tuft of hair, nevus, sinus, skin appendage, café-au-lait spots etc (Fig 5). A thorough neurologic assessment is performed including motor strength testing, sensory examination, deep tendon reflexes, abdominal reflexes (asymmetric or abnormal reflexes are reliable indicators of intraspinal pathology such as syringomyelia), plantar reflexes and clonus testing. Traditional teaching would state that any deviations from the usual clinical presentation or abnormal neurological findings are an indication for MRI evaluation of the spinal cord. However recent studies indicate that intraspinal anomalies can be present even in “typical” patients with AIS and hence MRI is preferred in all patients for medico-legal reasons.
Figure 4: Patient with right thoracic and left lumbar scoliosis that becomes manifest as right rib hump and left loin hump with forward bending
Figure 5: Posterior tuft of hair in the lumbo-sacral region
Radiographic assessment:
Radiographic assessment forms an important aspect of diagnosis, planning the management and assessing the prognosis of patients with AIS. A standing postero-anterior (PA) long cassette radiograph is the initial view obtained. Lateral radiographs are indicated when sagittal plane abnormalities are noted on physical examinations, for patients with back pain (when spondylolisthesis is suspected) and for pre-surgical planning prior to scoliosis correction. Supine side-bending radiographs are indicated for defining the curve type for pre-surgical planning prior to scoliosis surgery but are not required for a routine initial patient evaluation.
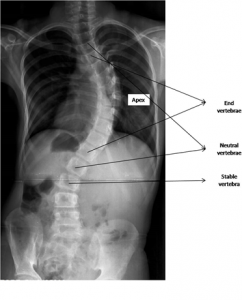
In the AP radiograph, the following radiographic parameters are studied, viz the end vertebra, apical vertebra, stable vertebra, neutral vertebra, curve location, curve direction, curve magnitude, and Risser sign.
End vertebra. The top and bottom vertebrae that tilt maximally into the concavity of the curve are termed as the end vertebra. They are typically the least rotated and least horizontally displaced vertebra within the curve
Apical vertebra: The apical vertebra is the central vertebra within a curve. It is typically the least tilted, most rotated, and most horizontally displaced vertebra within a curve
Neutral vertebra: As we move from the apical vertebra, the first distal vertebra that has no vertebral rotation is called as the neutral vertebra. In other words, the neutral vertebra is the first non-rotated vertebra at the caudal and cranial end of a curve. Rotation is assessed based on the radiographic appearance of the vertebral pedicle shadow in reference to the lateral margins of the vertebral body (Nash-Moe classification). In a neutrally rotated vertebra, the pedicle shadows will be equidistant from the lateral vertebral margins
Stable vertebra: As we move from the apical vertebra, the first distal vertebra which is bisected by the central sacral vertical line is called as the neutral vertebra
Curve direction: Curve direction is determined by the side of the convexity. Curves convex toward the right are termed right curves, while curves convex to the left are termed left curves
Curve location: The scoliotic curve is termed as cervico-thoracic, thoracic, thoraco-lumbar and lumbar based on its apex.
|
Curve |
Apex |
|
Cervicothoracic |
C7 or T1 |
|
Thoracic |
Between T2 and T11–T12 disc |
|
Thoracolumbar |
T12 or L1 |
|
Lumbar |
Between L1–L2 disc and L4 |
|
Lumbosacral |
L5 or S1 |
Figure 6: Radiographic assessment of scoliosis
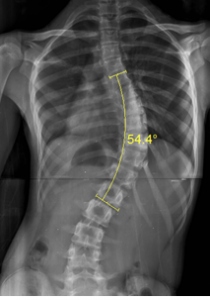
Curve magnitude: The Cobb technique is used to determine the curve magnitude. Perpendicular lines are drawn in relation to reference lines along the superior endplate of the upper end vertebra and along the inferior endplate of the lower end vertebra. The angle created by the intersection of the two perpendicular lines is termed the Cobb angle and defines the magnitude of the curve (Fig 7).
Figure 7: Measurement of Cobb angle between the end vertebrae
Risser sign: The Risser sign is used to assess the growth potential of the child. It describes the ossification of the iliac apophysis. Normally the iliac apophysis ossifies from lateral to medial. The iliac crest is divided into quarters (Fig 8), and the stage of ossification is used as a guideline to assess skeletal maturity: grade 0: absent, grade 1 (0–25%), grade 2 (26%–50%), grade 3 (51%–75%), grade 4 (76%–100%), grade 5 (fusion of apophysis to the ilium). Risser stages 0 and 1 indicate potential for high growth potential and rapid curve progression. Risser stage 4 correlates with the end of spinal growth in females, and Risser stage 5 correlates with the end of spinal growth in males.
Figure 8: Risser’s sign
Scoliosis classification:
King’s classification:
The King’s classification was the most commonly used classification before the advent of the Lenke’s classification. The King-Moe classification of thoracic curve patterns in idiopathic scoliosis distinguishes five curve types (Fig 9):
Figure 9: King’s classification – Types 1 to 5 (From Roach JW. Adolescent Idiopathic scoliosis. Orthop Clin North Am 1999;30:353-65)
Type 1: S-shaped curve in which both the thoracic and lumbar curves cross the midline. Both curves are structural, and the lumbar curve may be larger or less flexible than the thoracic curve
Type 2: S-shaped curve in which the thoracic curve is larger or less flexible than the lumbar curve (also called a “false” double major curve)
Type 3: Single thoracic curve without a structural lumbar curve
Type 4: Long thoracic curve in which L5 is centered over the sacrum and L4 is tilted into the thoracic curve
Type 5: Double thoracic curve with T1 tilted into the convexity of the upper curve
There are several inadequacies in the King’s classification. It does not address lumbar curves, thoracolumbar curves, or triple major curves. It does not evaluate sagittal plane alignment.
Lenke’s classification:
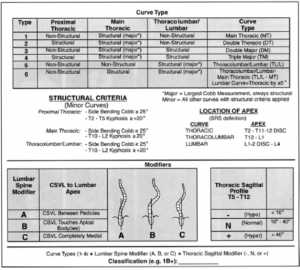
The Lenke classification was developed to overcome the pitfalls of King classification and is currently the most widely used classification. It is based on assessment of postero-anterior, lateral, and side-bending radiographs (Fig 10).
The basic steps in curve classification include three aspects:
Step 1: Determine curve type
Patients typically present with a combination of fixed and flexible spinal deformities. All curves are measured. The major curve is identified. The major curve is the curve with the largest Cobb measurement and is always a structural curve. All other curves are termed minor curves and may be either structural or non-structural, depending on classification criteria.
Determine whether the minor curves are structural or non-structural. Side-bending radiographs are used to assess the flexibility of curves. Curves that correct completely when the patient bends toward the convexity of the curve are termed non-structural curves. Non-structural curves permit the shoulders and pelvis to remain level to the ground and permit the head to remain centered in the midline above the pelvis. For this reason, nonstructural curves are also referred to as compensatory curves. Over time, compensatory curves may develop structural characteristics and become rigid. According to Lenke’s classification, curves that bend to less than 25 degrees are termed as non-structural curves.
Figure 10: Lenke classification. (From Hurley ME, Devlin VJ. Idiopathic scoliosis. In: Fitzgerald RH ed. Orthopaedics. St Louis: Mosby;2000)
Six curve types are identified:
• Primary thoracic
• Double thoracic
• Double major
• Triple major
• Primary thoracolumbar or lumbar
• Primary thoracolumbar or lumbar with a secondary thoracic curve
Step 2: Determine the lumbar spine modifier
The six main curve types are sub-classified as A, B, or C on relationship of the center sacral vertical line (CSVL) to the lumbar spine.
Step 3: Determine the thoracic sagittal modifier
“-”, “N”, or “1” is determined on, the T5 to T12 sagittal Cobb angle
This triad of radiographic information (curve type, lumbar modifier, sagittal modifier) is required to determine the curve classification (e.g. 1B1).
Treatment for scoliosis:
The treatment options for adolescent idiopathic scoliosis include observation, orthoses, and surgical treatment. There is no evidence that exercise programs, electrical stimulation, special diets, chiropractic adjustment, acupuncture, or other nontraditional treatment methods are effective in preventing curve progression or correcting established curves.
Several factors such as future growth potential of the patient (assessed by a variety of factors, including age at presentation, Risser stage, menarche, peak height velocity), curve magnitude at the time of diagnosis (> 40-50 degree curves are prone for progression), curve pattern (double curves progress more frequently than single curves), female sex (curves in females are more likely to progress than curves in males) and genetic risk score (ScoliScore Prognostic Test, Axial Biotech) are considered while managing patients with scoliosis.
Curves measuring less than 30° at maturity are least likely to progress. Curves measuring 30° to 50° degrees are likely to progress an average of 10° to 15° over the course of a normal lifetime. Curves measuring 50° to 75° at maturity progress steadily at a rate of approximately 1° per year. Lumbar and thoracolumbar curves are more likely to progress than thoracic curves because they lack the inherent stability provided by the rib cage.
Observation: The purpose of observation for adolescent idiopathic scoliosis is to identify and document curve progression and thereby facilitate timely intervention. Curves less than 20° are observed.
Bracing: Patients, who are Risser stage 0 to 1 and premenarchal, with curves 20° to 29° are candidates for immediate bracing. In the Risser stage 2 patient with a curve of 20° to 29°, progression of 5° should be documented before bracing is initiated. Patients presenting with curves of 30° to 40° should be braced immediately if they are skeletally immature. Patients and families should be advised that a spinal orthosis is used to prevent curve progression and generally does not lead to permanent curve improvement.
Contraindications to brace treatment include:
• Skeletally mature patients
• Curves greater than 40°
• Thoracic lordosis (bracing potentiates cardiopulmonary restriction)
• Patients unable to cope emotionally with treatment
The commonly used orthoses for adolescent idiopathic scoliosis are:
• Cervico-thoraco-lumbar sacral orthosis CTLSO (Milwaukee brace). Used less commonly due to its cosmetic appearance. However, for curves with an apex above T8, it is efficacious.
• Thoraco-lumbar sacral orthosis TLSO (e.g. Boston brace). These lower-profile orthoses are better accepted by patients and are indicated for curves with an apex at T8 or below
• Underarm brace (e.g. Charleston brace). This type of brace holds the patient is an acutely bent position in a direction opposite to the curve apex. It is worn only during sleep. It has been advocated as an alternative to full-time bracing regimens
Surgical treatment: In general, for the immature adolescent patient, surgery is indicated for curves greater than 40° that are progressive despite brace treatment. In the mature adolescent, surgery is considered for curves greater than 50°. The decision to operate is not based solely on the coronal Cobb angle alone and other factors that are considered include sagittal plane alignment, rotational deformity, the natural history of the patient’s curve, and skeletal maturity.
The possible treatment options include:
• Posterior spinal instrumentation and posterior fusion (commonly performed)
• Anterior spinal instrumentation and anterior fusion
• Anterior spinal fusion combined with posterior spinal instrumentation and fusion
Principles of surgical treatment:
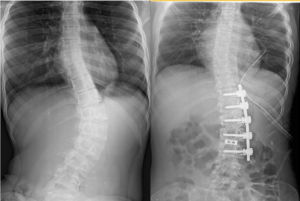
Posterior technique:
Figure 11: Posterior corrective fusion for Lenke Type 1B curve
The posterior surgical approach is applicable to all idiopathic scoliosis curve types (Fig 11). During the surgical procedure, the posterior spinal structures are exposed sub-perisoteally. After inserting pedicle screws either segmentally or strategically, the facet joints, inter-spinous and supraspinous ligaments are excised to ‘loosen’ the curve. Contoured rods are placed into the screws and the deformity is corrected. Posterior spinal elements are decorticated and local autografts are packed into the facet joints and posterior elements. Instead of all-pedicle screws, hybrid constructs with a combination of hooks, wires (cables), and/or pedicular screws can also be used.
Anterior techniques:
Anterior spinal instrumentation and fusion procedures are most commonly indicated for single thoracic, thoracolumbar, or lumbar curve types (Fig 12). The convex side of the curve is exposed. The thoracic spine is approached via thoracotomy and the disc, annulus, and cartilaginous vertebral endplates are excised over the levels undergoing fusion. Screws are inserted into vertebral body and deformity is corrected. The disc spaces are packed with non-structural bone graft. Structural spacers are placed in the disc spaces in the lumbar region.
Figure 12: Anterior scoliosis correction for Lenke Type 5C curve
With the use of modern segmental pedicle screw instrumentation and different posterior spinal osteotomies such as Smith-Petersen osteotomies, Ponte osteotomies and posterior vertebral column resection procedures, most severe curves can be treated with a single-stage posterior approach. Combined anterior and posterior spinal procedures for adolescent idiopathic scoliosis are rarely required for uncomplicated adolescent idiopathic scoliosis. Circumstances where combined anterior and posterior procedures are occasionally considered include extremely large stiff curves, presence of coexistent rigid sagittal plane deformities (e.g. excessive thoracic lordosis, hyperkyphosis), prevent the crankshaft phenomenon in young patients with severe curves and revision procedures following unsuccessful prior scoliosis surgery.
| Frequently Asked Questions in Scoliosis Treatment! |
1. What is the earliest sign of neurological involvement in scoliosis
– asymmetric abdominal reflex – suspect syringx.
2. When does peak height velocity occur during growth ?
– occurs before risser grade i or just before the onset of menses.
3. What are the long term implications of ai scoliosis –
- thoracic curve less than 50 deg and lumbar cuves less than 40 degrees most often progress at the rate of 1deg/year.
- curves greater than 60 deg – has a negative impact on cardiopulmonary status
4. When is MRI indicated in scoliosis-
- Atypical curves – left thoracic curves , angular curves, congenital scoliosis, absence of thoracic lordosis.
- Presence of neurocutanoeus markers – hairy patches, cafe au lait spots, dimples, nevi.
- Patients less than 10 years of age with 20 degree curves.
- Rapid progression of the curve.
5. What is the aim of bracing in scoliosis – bracing halts the progression of scoliosis while it does not correct the pre exiting deformity in contradiction to its use for kyphosis.
6. What are the contraindications for bracing?
– children less than 2 years,
– thoracic hypokyphosis,
– curves more than 25 deg ,
– rapid progression of the curve
– congenital curves.
Ref:
- King HA, Moe JH, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg 1983;65A:1302–13.
- Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis—a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg 2001;83A:1169–81.
- Lenke LG, Kuklo TR, Ondra S, et al. Rationale behind the current state of the art treatment of scoliosis in the pedicle screw era. Spine 2008;33:1051–4.
- Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg 1984;66A:1061–71.
- Sanders JO. Maturity indicators in spinal deformity. J Bone Joint Surg 2007;89A:S14–S20.
- Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine 2005;30:1602-9





sir,
kindly send me the full article of ideopathic scoliosis.
i will be highly obliged.
regards
Very impressive article.