MORRANT BAKER’S CYST (BAKER’S CYST)
Aetiopathogenesis:
• “A type of cyst which results from egress of fluid through a normal communication of a bursa (semimembranosus or medial gastrocnemius bursa) or caused by herniation of the synovial membrane through the joint capsule”- Mayerding and Van Denmark
• Named after Baker (described it in 1877), though Adams had described it earlier in 1840.
• Symptoms develop in the bursa beneath the medial head of the gastrocnemius or in the semimembranosus bursa
• It develops due to chronic irritation, that increases the production of synovial fluid and distends one of the six bursae, commonly the medial gastrocnemius-semi membranous bursa
• Chronic irritation is commonly due to osteoarthritis or rheumatoid arthritis
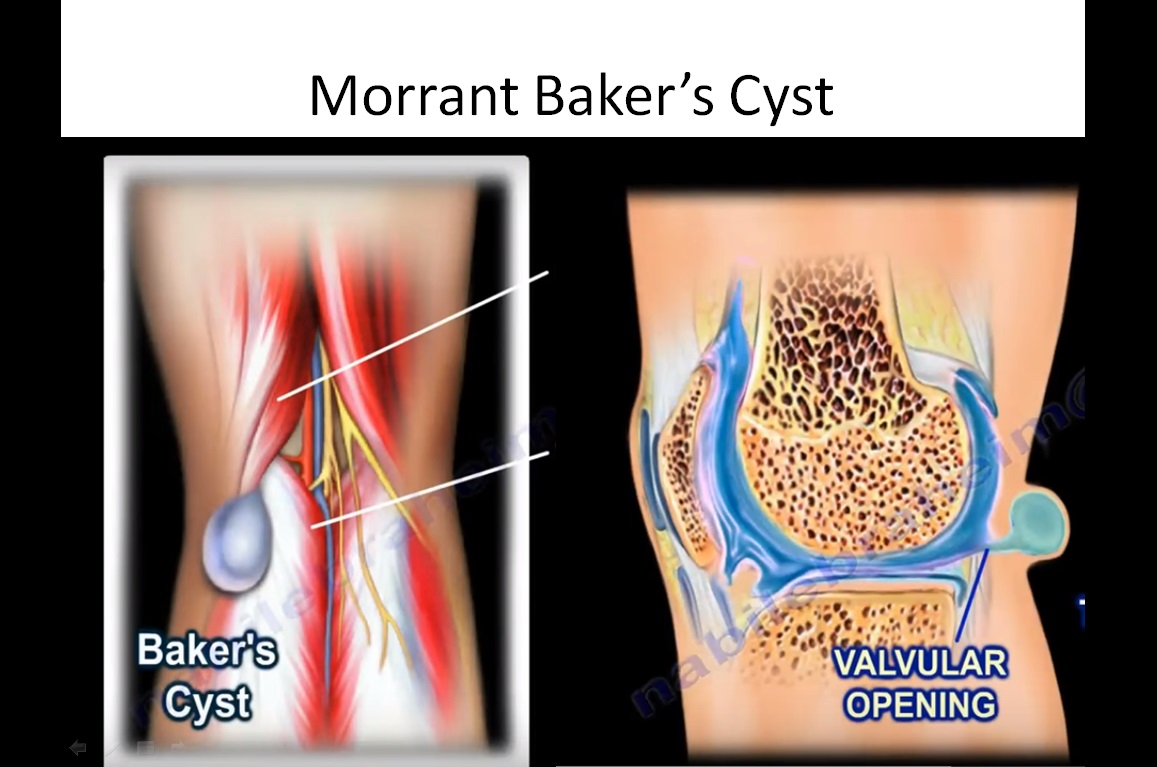
• Cysts are connected to the knee joint through valvular opening.
• More common in adults than in children
• The aetiology for Popliteal cysts differ in children and adults
• An underlying intraarticular pathology is rare in children whereas in an adult an intraarticular pathology is usually evident (e.g., patellofemoral Chondromalacia or a degenerative tear of the posterior horn of the medial meniscus)
• Hence in adults the intraarticular pathology should be concurrently treated or it may recur.
• A dissecting popliteal cyst can be the presenting feature of a malfunctioning total knee arthroplasty
Clinical Features:
• The popliteal cyst always transilluminates, often lying on the medial side of the popliteal fossa
• Foucher’s sign: with the patient prone, and the knee extended the swelling will appear prominent, but with knee flexion the swelling becomes soft and less prominent
• The cyst can extend into the thigh or legs and can have multiple satellite cysts all along the leg, which may or may not be connected
• A dissecting popliteal cyst may mimic acute thrombophlebitis (or deep vein thrombosis), where the calf is painful and swollen, and the Homan sign is positive-“pseudothrombophlebitis syndrome”
• Rarely, a dissecting popliteal cyst may coexist with popliteal vein thrombosis
• Rarely can cause compartment syndrome, peripheral neuropathy, calf, foot and ankle ecchymoses, septic arthritis of the knee if it gets infected.
Investigations:
• X-rays should be taken to rule out other causes of swelling in the popliteal fossa. For e.g., soft tissue calcifications may indicate the presence of a synovial sarcoma or a hemangioma
• Aspiration confirms the diagnosis. Always rule out a vascular malformation from the popliteal artery prior to aspiration by auscultation for a bruit.
• Ultrasound helps to differentiate a cyst from other causes of swelling in the popliteal space (e.g., lipoma, xanthoma, vascular tumor, Fibrosarcoma)
• MRI and Arthrography also helps in establishing a diagnosis
Treatment:
• In children the cyst spontaneously resolves.
• In adults the cyst may be excised and the underlying pathology may be treated to
decrease the incidence of recurrence
• Arthroscopy should be performed prior to excision of popliteal cyst (patellofemoral chondromalacia or a degenerative tear of the posterior horn of the medial meniscus may be treated prior to excision of cyst)
• Hughston, Baker, and Mello’s posteromedial approach: made through a medial hockey-stick incision for excision of the cyst
Ref:
1. Dirschl DR, Lachiewicz PF: Dissecting popliteal cyst as the presenting symptom of a malfunctioning total knee arthroplasty: a report of four cases. J Arthroplasty 1992; 7:37
2. Ko SH, Ahn JH: Popliteal cystoscopic excisional debridement and removal of capsular fold of valvular mechanism of large recurrent popliteal cyst. Arthroscopy 2004; 20:37.
3. Meyerding HW, Van Demark RE: Posterior hernia of the knee (Baker’s cyst, popliteal cyst, semimembranosus bursitis, medial gastrocnemius bursitis and popliteal bursitis). JAMA 1943; 122:858
4. Takahashi M, Nagano A: Arthroscopic treatment of popliteal cyst and visualization of its cavity through the posterior portal of the knee. Arthroscopy 2005; 21:638.
5. Curl WW: Popliteal cysts: historical background and current knowledge. J Am Acad Orthop Surg 1996; 4:129.
-the term ‘cyst’ is a misnomer because it is not a true cyst but in fact a distention of the gastrocnemius-semimembranosus bursa bulging from the back of the joint. (john hardy. popliteal cyst in adults)
-male to female ratio 2:1. two age-incidence peaks observed in patients with politeal cysts – first one from 4 to 7 years and the other from 35 to 70 years
-classified anatomically and clinically as
–primary – there is no communication between the distension of the bursa and the knee joint, no associated knee derangement, majority are seen in children.
–secondary – communicates freely between the bursa and the knee joint, almost all popliteal cysts are secondary.
-Adults may complain of a swelling, a mass, pain, or stiffness which worsen by activity
– in children its an incidental finding.
-physical examination may miss a popliteal cyst. Identification of fluid between the semimembranosus and medial gastrocnemius tendons in communication in Ultrasound is diagnostic.
-Communication between the posterior knee joint and the gastrocnemiosemimembranosus bursa has been shown to increase with age, possibly because of degenerative thinning of the joint capsule compounded by joint effusion and increased intraarticular pressure associated with internal derangement.
Fluid within a Baker’s cyst may communicate freely with the knee joint. However, the presence of a valvelike mechanism may allow joint fluid to communicate in only one direction.